
Chronic Obstructive Pulmonary Disease and Arthritis Among US Adults, 2016
ORIGINAL RESEARCH — Volume 16 — July 18, 2019
Yong Liu, MD, MS1; Anne G. Wheaton, PhD1; Louise B. Murphy, PhD1; Fang Xu, PhD1; Janet B. Croft, PhD1; Kurt J. Greenlund, PhD1 (View author affiliations)
Suggested citation for this article: Liu Y, Wheaton AG, Murphy LB, Xu F, Croft JB, Greenlund KJ. Chronic Obstructive Pulmonary Disease and Arthritis Among US Adults, 2016. Prev Chronic Dis 2019;16:190035. DOI: http://dx.doi.org/10.5888/pcd16.190035.
PEER REVIEWED
On This Page
Summary
What is already known on this topic?
More than 54 million US adults report having arthritis, and more than 15 million US adults report having chronic obstructive pulmonary disease.
What is added by this report?
Adults with arthritis are more likely than adults without arthritis to have a higher prevalence of COPD (13.7% vs 3.8%). The relationships remained significant among all subgroups of selected characteristics after we controlled for covariates.
What are the implications for public health practice?
Assessment of COPD and arthritis symptoms by health care providers may enhance earlier detection of each condition. Evidence-based self-management programs may ameliorate symptoms.
Abstract
Introduction
More than 54 million US adults have arthritis, and more than 15 million US adults have chronic obstructive pulmonary disease (COPD). Arthritis and COPD share many risk factors, such as tobacco use, asthma history, and age. The objective of this study was to assess the relationship between self-reported physician-diagnosed COPD and arthritis in the US adult population.
Methods
We analyzed data from 408,774 respondents aged 18 or older in the 2016 Behavioral Risk Factor Surveillance System to assess the association between self-reported physician-diagnosed COPD and arthritis in the US adult population by using multivariable logistic regression analyses.
Results
Overall crude prevalence was 6.4% for COPD and 25.2% for arthritis. The prevalence of age-adjusted COPD was higher among respondents with arthritis than among respondents without arthritis (13.7% vs 3.8%, P < .001). The association remained significant among most subgroups (P < .001) particularly among adults aged 18 to 44 (11.5% vs 2.0%) and never smokers (7.6% vs 1.7%). In multivariable logistic regression analyses, arthritis status was significantly associated with COPD status after controlling for sociodemographic characteristics, risk behaviors, and health-related quality of life measures (adjusted prevalence ratio = 1.5, 95% confidence interval, 1.4–1.5, P < .001).
Conclusion
Our results confirmed that arthritis is associated with a higher prevalence of COPD in the US adult population. Health care providers may assess COPD and arthritis symptoms for earlier detection of each condition and recommend that patients with COPD and/or arthritis participate in pulmonary rehabilitation and self-management education programs such as the Chronic Disease Self-Management Program, the proven benefits of which include increased aerobic activity and reduced shortness of breath, pain, and depression.
Introduction
More than 15 million US adults have chronic obstructive pulmonary disease (COPD), and more than 54 million US adults have arthritis (1,2). COPD is characterized by progressive, irreversible airflow limitation and was the fourth leading cause of death in the United States in 2016 (3). Arthritis is a common chronic condition and a leading cause of disability (4). Data from cross-sectional studies suggest that adults with COPD are more likely than adults without COPD to have arthritis (5), including osteoarthritis (6) and rheumatoid arthritis (7). Emerging evidence from longitudinal studies also shows a higher risk of developing COPD among adults with arthritis than adults without arthritis at baseline (8–11). COPD and arthritis share many of the same risk factors, such as sex, age, lower socioeconomic status, tobacco use, obesity, and infection (12–14). Most previous studies assessed the COPD–arthritis relationship by controlling for those common risk factors (9–11). However, few studies, including nationally representative studies, examined the relationship among subgroups with or without those risk factors (5,11). Describing these relationships may inform health care providers to assess COPD and arthritis symptoms for earlier detection of these conditions and provide new insights into preventing them.
The objective of this study was to assess the relationship between self-reported physician-diagnosed COPD and arthritis in the US adult population aged 18 or older in the 2016 Behavioral Risk Factor Surveillance System (BRFSS). We examined the relationship among subgroups with and without the common risk factors.
Methods
The BRFSS is a random-digital–dialed landline and cellular telephone survey that is conducted by state health departments in collaboration with the Centers for Disease Control and Prevention (CDC) in all 50 states, the District of Columbia, and US territories (www.cdc.gov/brfss). The BRFSS collected data on sociodemographic characteristics, health-related behaviors, chronic diseases, and other conditions among the adult population (aged ≥18) in 2016. Disproportionate stratified sampling of respondents defined by race/ethnicity, sex, or age may vary between states. CDC weighted each sample using design weighting and “raking” weighting methods to obtain a study population representative of each state. Trained interviewers administered standardized questionnaires to all adult respondents. All respondents provided an oral consent statement for participating in the survey. The study was approved as exempt research by CDC’s institutional review board.
Measures
Respondents who answered yes to the question of whether they had ever been told by a doctor, nurse, or other health professional that they had “chronic obstructive pulmonary disease (COPD), emphysema, or chronic bronchitis” or arthritis (“some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia”) were determined to have those conditions. Asthma status, a covariable in this study, was based on questions about whether respondents had ever been told they had asthma and “still have asthma.” We categorized responses as current asthma, history of asthma only, or no asthma.
Other covariates were age groups (18–44, 45–64, 65–74, and ≥75 y), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, American Indian/Alaska Native, Asian, and non-Hispanic other), education levels (<high school diploma, high school diploma or GED, some college, and college graduate), and employment status (employed, unemployed, retired, unable to work, and other). Sleep duration was defined according to a response to the question, “On average, how many hours of sleep do you get in a 24-hour period?” We defined short sleep duration as fewer than 7 hours of sleep (15). The number of physically unhealthy days was determined according to the question, “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?” The number of mentally unhealthy days was determined according to the question, “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” Consistent with previous research (16), frequent physical distress was defined as 14 or more physically unhealthy days, and frequent mental distress was defined as 14 or more mentally unhealthy days. Any leisure-time physical activity was defined according to a yes response to a single question, “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?” Smoking status was defined by 2 questions: “Have you smoked at least 100 cigarettes in your entire life?” and “Do you currently smoke every day, some days, or not at all?” Respondents were current smokers if they reported having smoked at least 100 cigarettes during their lifetime and currently smoked every day or some days. Former smokers were defined as respondents who reported having smoked at least 100 cigarettes during their lifetime but did not currently smoke. Never smokers were defined as respondents who reported not having smoked at least 100 cigarettes during their lifetime. Body mass index (BMI, kg/m2) was calculated from self-reported height and weight and categorized as underweight (BMI < 18.5), normal weight (BMI = 18.5–24.9), overweight (BMI = 25.0–29.9), or obese (BMI ≥ 30.0). Excessive alcohol drinkers were defined as respondents who had any alcohol drinks and were younger than 21, women who were pregnant and reported drinking any alcohol in the previous month, or respondents who were binge drinkers (≥5 drinks for men on an occasion and ≥4 drinks for women on an occasion) or heavy drinkers (≥15 drinks per week for men and ≥8 drinks per week for women during the past 30 days) (17).
In 2016, 486,303 respondents aged 18 or older residing in 50 states, Washington, DC, and the US territories participated in the survey. The median response rate was 47.1% (range, 30.7% in Louisiana to 65.0% in Wyoming) (18). After we excluded respondents with missing values (age [n = 6,697], COPD [n = 156], arthritis [n = 99], or risk behaviors and health-related quality of life [n = 70,577]), we analyzed complete data for 408,774 adult respondents.
Statistical analysis
We calculated the age-adjusted prevalence of COPD and 95% confidence intervals (CIs) by standardizing to the 2000 projected US population in 5 age groups (18–24, 25–34, 35–44, 45–64, and ≥ 65) by arthritis status and selected characteristics (19). We performed multivariable logistic regression analyses to assess the association of COPD with arthritis after controlling for age, sex, race/ethnicity, education levels, employment status, short sleep duration, frequent mental distress, frequent physical distress, smoking status, BMI category, leisure-time physical activity, excessive alcohol drinking, and asthma status. We conducted all analyses in SAS–callable SUDAAN version 11.0.1 (Research Triangle Institute) to account for the complex sampling design. We determined significant differences at P < .05.
Results
Respondents with arthritis were more likely than respondents without arthritis to be women, aged 45 or older, non-Hispanic white, and not a college graduate, to be retired or unable to work, to have frequent mental or physical distress, to be former or current smokers, to have short sleep duration, to be obese, and to have current asthma or a history of COPD. Respondents with arthritis were less likely than respondents without arthritis to report excessive alcohol drinking or leisure-time physical activity (P < .001) (Table 1).
The crude prevalence of COPD and arthritis was 6.4% and 25.2%, respectively, among US adults in 2016. Respondents with arthritis had a higher age-adjusted COPD prevalence than respondents without arthritis overall (13.7% vs 3.8%, P < .001) (Table 2). In subgroup analyses, we observed a higher prevalence of COPD and arthritis with increasing age (Figure 1).
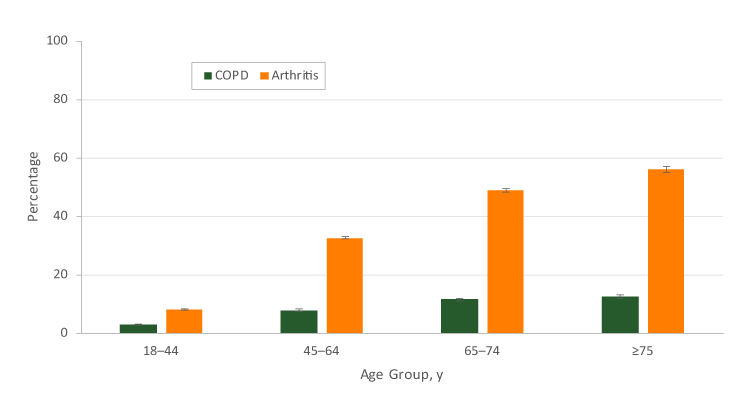
Figure 1.
Age-specific percentage of self-reported chronic obstructive pulmonary disease (COPD) and arthritis among US adults aged ≥18, 2016 Behavioral Risk Factor Surveillance System. Error bars indicate standard errors. [A tabular version of this figure is also available.]
Age-specific percentage of self-reported chronic obstructive pulmonary disease (COPD) and arthritis among US adults aged ≥18, 2016 Behavioral Risk Factor Surveillance System. Error bars indicate standard errors. [A tabular version of this figure is also available.]
The age-adjusted prevalence of COPD was higher among respondents with arthritis than among respondents without arthritis, regardless of sex, age group, education level, employment status, frequent mental distress, frequent physical distress, leisure-time physical activity, smoking status, short sleep duration, BMI category, excessive alcohol drinking, and asthma status (P < .001) (Table 2). The age-adjusted prevalence of COPD was higher among respondents with arthritis than among respondents without arthritis in most racial/ethnic groups (P< .001). Although the prevalence of COPD was low in some subgroups (eg, younger adults, college graduates, and respondents who never smoked), respondents with arthritis were significantly more likely than respondents without arthritis to report COPD in these subgroups. For example, among adults aged 18 to 44, the age-adjusted prevalence of COPD was 11.5% for respondents with arthritis and 2.0% for respondents without arthritis (Figure 2).
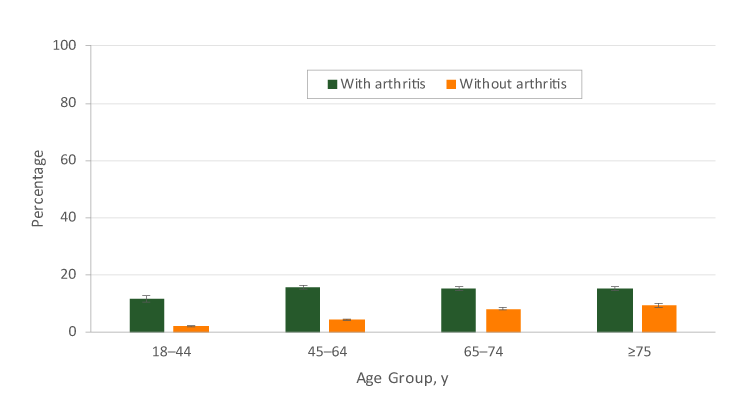
Figure 2.
Age-specific prevalence of chronic obstructive pulmonary disease (COPD) among US adults aged ≥18 years, by arthritis status, 2016 Behavioral Risk Factor Surveillance System. Error bars indicate standard errors. [A tabular version of this figure is also available.]
Age-specific prevalence of chronic obstructive pulmonary disease (COPD) among US adults aged ≥18 years, by arthritis status, 2016 Behavioral Risk Factor Surveillance System. Error bars indicate standard errors. [A tabular version of this figure is also available.]
Among never smokers, the prevalence of COPD was 7.6% for respondents with arthritis and 1.7% for respondents without arthritis (Figure 3).
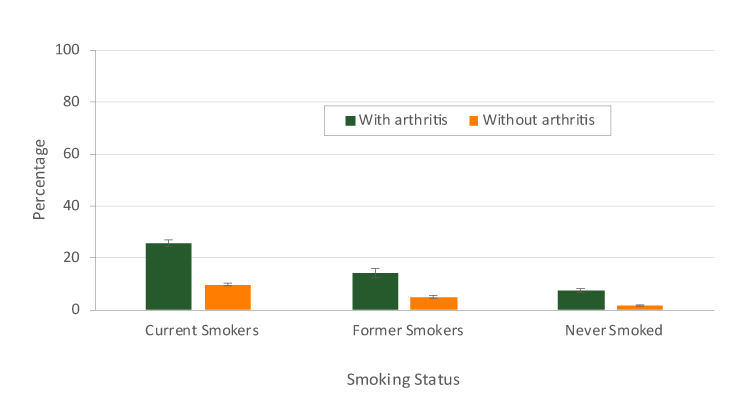
Figure 3.
Age-adjusted prevalence of chronic obstructive pulmonary disease (COPD) among US adults aged ≥18 years, by smoking status and arthritis, 2016 Behavioral Risk Factor Surveillance System. Error bars indicate standard errors. [A tabular version of this figure is also available.]
Age-adjusted prevalence of chronic obstructive pulmonary disease (COPD) among US adults aged ≥18 years, by smoking status and arthritis, 2016 Behavioral Risk Factor Surveillance System. Error bars indicate standard errors. [A tabular version of this figure is also available.]
In multivariable logistic regression analyses, arthritis was significantly associated with COPD, after controlling for sociodemographics, risk behaviors, frequent mental distress, frequent physical distress, and asthma status (adjusted prevalence ratio = 1.5, 95% confidence interval, 1.4–1.5; P < .001) (Table 2). The association remained statistically significant among most subgroups by selected characteristics, including adults aged 18 to 44 and nonsmokers.
Discussion
Our study demonstrated that the prevalence of COPD was almost 50% higher among adults with arthritis than among adults without arthritis in the United States after adjustment for sociodemographic characteristics, risk behaviors, frequent mental distress, frequent physical distress, and asthma status. Additionally, the relationship between COPD and arthritis was evident in essentially all subgroups of sociodemographic characteristics, risk behaviors, frequent mental distress, frequent physical distress, and a history of asthma. Our results, from a large nationwide sample, are consistent with the results of previous hospitalization and clinical studies of the association between COPD and osteoarthritis or rheumatoid arthritis (5–11). Those previous studies showed only the association between COPD and arthritis in sex and age groups (5,7,8,10,11). Therefore, our results add epidemiological information to the existing literature.
The reason for a positive association between COPD and arthritis is not clear. First, prolonged systemic inflammation may mediate the relationship between arthritis and COPD (8). Second, smoking is a common risk factor for both arthritis and COPD, and it may exacerbate the 2 underlying conditions (20,21). Therefore, smoking cessation is important to preventing and managing arthritis and COPD. Third, stiff joints and joint pain, weak muscles, and poor balance are common symptoms of arthritis. These symptoms can limit a person’s physical activity and further impair respiratory function in people who also have COPD. Conversely, dyspnea or shortness of breath are common symptoms of COPD and can make arthritis worse if patients become more sedentary (22). Therefore, physical inactivity may contribute to the relationship between COPD and arthritis. However, aerobic activity could reduce symptoms of both COPD and arthritis (22,23). Therefore, aerobic physical activity interventions or pulmonary rehabilitation may improve long-term health outcomes for patients with COPD and/or arthritis (22,23). Finally, follow-up care and treatment of one condition may lead health care providers to detect and diagnose comorbid conditions.
Our study showed that the greater prevalence of COPD among adults with arthritis than among adults without arthritis remained significant among all subgroups by selected characteristics in multivariable logistic regression models including sociodemographics, risk behaviors, frequent mental distress, frequent physical distress, and asthma status. It also demonstrated that the relationship between COPD and arthritis was not only among people with common risk factors but also among younger adults and among nonsmokers. Our findings imply that assessment of COPD and arthritis symptoms by a primary care physician might be advised for persons with arthritis or COPD.
Health care providers may also consider referring their patients to evidence-based self-management education programs, such as the Chronic Disease Self-Management Program (CDSMP), which were developed to help people with chronic diseases such as COPD and arthritis manage their symptoms and improve their quality of life (24). A meta-analysis showed that people participating in CDSMP experienced numerous benefits, including reduced shortness of breath, pain, and depression and increased aerobic activity (25).
Our study had several limitations. First, because BRFSS is a cross-sectional survey, we cannot make causal inferences. Second, arthritis was defined as a broad category that included rheumatoid arthritis, gout, lupus, fibromyalgia, or any other form of arthritis. There are more than 100 types of arthritis (26), and our results may not apply to all types. Further research on associations between COPD and various types of arthritis may reveal more insights into the relationship. Third, sample selection bias due to low response rates may have also influenced our results. However, the effect of potential systematic bias was likely limited because the relationship between COPD and arthritis in our study is consistent with the relationship described in previous studies (5,8). Finally, all responses to survey questions in the study were self-reported; as such, they were subject to recall bias, and this bias might have affected our results.
Our results confirmed that arthritis was associated with a higher likelihood of COPD in the US adult population. Health care providers may assess COPD and arthritis symptoms for earlier detection and recommend to their patients with COPD and/or arthritis to participate in evidence-based self-management education programs such as the Chronic Disease Self-Management Program to manage their symptoms, including shortness of breath, pain, and depression, and improve their quality of life.
Acknowledgments
This research received no grant from funding agencies in the public, commercial, or nonprofit sectors. No copyrighted surveys, instruments, or tools were used. We acknowledge Dr. Youlian Liao’s valuable comments on the manuscript (Office of Director, Division of Population Health, CDC). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC.
Author Information
Corresponding Author: Yong Liu, MD, MS, Division of Population Health, Centers for Disease Control and Prevention, 4770 Buford Hwy, Mail Stop S107-6, Atlanta, Georgia 30341. Telephone: 770-488-5528. Email: ikd8@cdc.gov.
Author Affiliations: 1Division of Population Health, Centers for Disease Control and Prevention, Atlanta, Georgia.
References
- Croft JB, Wheaton AG, Liu Y, Xu F, Lu H, Matthews KA, et al. Urban-rural county and state differences in chronic obstructive pulmonary disease — United States, 2015. MMWR Morb Mortal Wkly Rep 2018;67(7):205–11. CrossRef PubMed
- Barbour KE, Helmick CG, Boring M, Brady TJ. Vital signs: prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation — United States, 2013–2015. MMWR Morb Mortal Wkly Rep 2017;66(9):246–53. CrossRef PubMed
- Heron M. Deaths: leading causes for 2016. National Vital Statistics Reports. Vol 67, no 6. Hyattsville (MD): National Center for Health Statistics; 2018. https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_06.pdf. Accessed May 1, 2018.
- Centers for Disease Control and Prevention (CDC). Prevalence and most common causes of disability among adults — United States, 2005. MMWR Morb Mortal Wkly Rep 2009;58(16):421–6. PubMed
- Schnell K, Weiss CO, Lee T, Krishnan JA, Leff B, Wolff JL, et al. The prevalence of clinically-relevant comorbid conditions in patients with physician-diagnosed COPD: a cross-sectional study using data from NHANES 1999–2008. BMC Pulm Med 2012;12(1):26. CrossRefPubMed
- Wshah A, Guilcher SJT, Goldstein R, Brooks D. Prevalence of osteoarthritis in individuals with COPD: a systematic review. Int J Chron Obstruct Pulmon Dis 2018;13:1207–16. CrossRef PubMed
- Bieber V, Cohen AD, Freud T, Agmon-Levin N, Gertel S, Amital H. Autoimmune smoke and fire — coexisting rheumatoid arthritis and chronic obstructive pulmonary disease: a cross-sectional analysis. Immunol Res 2013;56(2-3):261–6. CrossRef PubMed
- Mcguire K, Aviña-Zubieta JA, Esdaile JM, Sadatsafavi M, Sayre EC, Abrahamowicz M, et al. Risk of incident chronic obstructive pulmonary disease (COPD) in rheumatoid arthritis: a population based cohort study. Arthritis Care Res (Hoboken) 2017. PubMed
- Sparks JA, Lin TC, Camargo CA Jr, Barbhaiya M, Tedeschi SK, Costenbader KH, et al. Rheumatoid arthritis and risk of chronic obstructive pulmonary disease or asthma among women: a marginal structural model analysis in the Nurses’ Health Study. Semin Arthritis Rheum 2018;47(5):639–48. CrossRef PubMed
- Ursum J, Nielen MM, Twisk JWR, Peters MJL, Schellevis FG, Nurmohamed MT, et al. Increased risk for chronic comorbid disorders in patients with inflammatory arthritis: a population based study. BMC Fam Pract 2013;14(1):199. CrossRef PubMed
- Shen TC, Lin CL, Chen CH, Tu CY, Hsia TC, Shih CM, et al. Increased risk of chronic obstructive pulmonary disease in patients with rheumatoid arthritis: a population-based cohort study. QJM 2014;107(7):537–43. CrossRef PubMed
- Alamanos Y, Drosos AA. Epidemiology of adult rheumatoid arthritis. Autoimmun Rev 2005;4(3):130–6. CrossRef PubMed
- Allen KD, Golightly YM. State of the evidence. Curr Opin Rheumatol 2015;27(3):276–83. CrossRef PubMed
- Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet 2007;370(9589):765–73. CrossRefPubMed
- Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015;38(6):843–4. PubMed
- Shockey TM, Zack M, Sussell A. Health-related quality of life among US workers: variability across occupation groups. Am J Public Health 2017;107(8):1316–23. CrossRef PubMed
- US Department of Health and Human Services and US Department of Agriculture. 2015−2020 Dietary guidelines for Americans, 8th ed. 2015. https://health.gov/dietaryguidelines/2015/guidelines.
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. 2016 Summary data quality report; June 29, 2017. https://www.cdc.gov/brfss/annual_data/2016/pdf/2016-sdqr.pdf. Accessed May 1, 2018.
- Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People Stat Notes 2001(20):1–10.
- Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007;176(6):532–55. CrossRef PubMed
- Arnson Y, Shoenfeld Y, Amital H. Effects of tobacco smoke on immunity, inflammation and autoimmunity. J Autoimmun 2010;34(3):J258–65. CrossRef PubMed
- Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013;188(8):e13–64. CrossRefPubMed
- Pinto AJ, Roschel H, de Sá Pinto AL, Lima FR, Pereira RMR, Silva CA, et al. Physical inactivity and sedentary behavior: overlooked risk factors in autoimmune rheumatic diseases? Autoimmun Rev 2017;16(7):667–74. CrossRef PubMed
- Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW Jr, Bandura A, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care 2001;39(11):1217–23. CrossRef PubMed
- Brady TJ, Murphy L, O’Colmain BJ, Beauchesne D, Daniels B, Greenberg M, et al. A meta-analysis of health status, health behaviors, and health care utilization outcomes of the Chronic Disease Self-Management Program. Prev Chronic Dis 2013;10:120112. CrossRefPubMed
- Arthritis Foundation. What is arthritis? https://www.arthritis.org/about-arthritis/understanding-arthritis/what-is-arthritis.php. Accessed March 5, 2019.
No hay comentarios:
Publicar un comentario