
A 'Pharmacy Phamily' team effort recognized at Naval Hospital Bremerton

Pharmacy technician Hospital Corpsman 3rd Class Shealie Brown fills a prescription order in Naval Hospital Bremerton's Inpatient Pharmacy, part of the command's Pharmacy Department that along with Branch Health Clinics (BHC) Bangor, Everett and Puget Sound Naval Shipyard (PSNS) pharmacies, has been selected for the 2018 Navy Pharmacy Team Award. (U.S. Navy photo by Douglas Stutz)
There might not be an ‘I’ in team, but there is a ‘ph’ in family with Naval Hospital Bremerton’s (NHB) Pharmacy.
That notion of ‘phamily’ is the primary reason why NHB’s Pharmacy, which includes Branch Health Clinics (BHC) Bangor, Everett and Puget Sound Naval Shipyard (PSNS), has been selected for the 2018 Navy Pharmacy Team Award.
“This was truly a team effort. Truly no one individual can take the credit. The ‘phamily’ came together to ensure the success of the pharmacy and the best care possible to our patients,” explained Navy Lt. Cmdr. Dean Kang, NHB Pharmacy Department head.
There were overlapping trials and tribulations – primarily an intensive renovation project and the deployment of the Department of Defense’s new electronic health record (EHR) MHS GENESIS – over the last fiscal year that the entire staff had to handle which actually brought them even closer together than before as a team.
With NHB identified as one of the Initial Operating Capability test sites for MHS GENESIS, the pharmacy was charged with consolidating multiple legacy medical informatics systems into a single integrated EHR to process inpatient and outpatient pharmacy services. There were glitches identified in training and workflow challenges, as well as a host of medication/formulary modifications that had to be updated. The driving theme behind such attention to detail during the roll out was patient safety.
“Patient safety has always remained our number one priority. During the most trying periods of our remodel and our initial implementation of MHS GENESIS, part of the reason our delays became exceedingly high were due to the fact that we needed to ensure the patient was still getting safe care. During the early stages, it unfortunately came at the sacrifice of wait times,” Kang stated.
The renovation project included doubling the window operating capacity from six to 12, increasing shelf space by more than 50 percent, reconfiguring the outpatient pharmacy work area, and adding new pharmacists and pharmacy technicians.
For pharmacy technician Hospital Corpsman 3rd Class Shealie Brown, her command being acknowledged as the top Navy Pharmacy Team for 2018 was validation for their effort during the past year.
“It feels good for us all to be recognized for what we do, and for what we went through for months and months. We were a ‘phamily.’ Everyone was checking on everyone else. There was a lot care and concern for others. Even our trainers became a part. It did feel like everything piled on at once. There were times we weren’t sure when we’d leave. I remember one time we had 96 people waiting in outpatient pharmacy for their prescriptions. But we were not going to leave until everyone got their medications. It took a long time there for a while until we got it all worked out,’ related Brown.
“Our goal has always been to give our patients the best service, in the timeliest manner, as we can. The ongoing construction and the new electronic health record did slow our services. Some of our patients were understandable about the delay in getting their orders processed but some weren’t. We understood their frustration because we also felt the same. There were some mornings where we would have people lined up an hour before we opened to get their tracking ticket trying to avoid a possible wait of several hours. Those were our dark days. When we added new staff, opened more windows, and got better hands-on with MHS GENESIS, it really greatly improved our service,” added Hospital Corpsman 2nd Class Seth Meshach, pharmacy technician.
Going through those dark days did have a positive. It brought the entire pharmacy team together to weather the storm of frustration.
“There just was this team mentality that developed. We could tell when someone needed a break. We would step in. We learned the new system, adapted to dealing in a stressful environment, and we still managed to smile,” Meshach said.
And the ‘pharmacy phamily’ nickname?
“I think it’s great. Being away from home in the Navy, this is like my second family. I completely embrace the concept and enjoy it,” said Meshach.
The prescription numbers alone are a testament to the pharmacy’s continual team effort. From January through September 22, 2017, there were 489,181 outpatient prescriptions filled – with 28,057 at BHC Bangor, 44,741 at BHC Everett and 1,113 at BHC PSNS – and another 75,526 inpatient medications orders verified. On a daily basis, there was an average of over 2,390 prescriptions and medication orders processed, along with providing around-the-clock service to NHB’s Urgent Care Clinic, Labor and Delivery, and Multi-Service Unit.
Additionally, the pharmacy team further defined the position description of Navy Medicine’s ‘Navy Comprehensive Pain Management Program’ by originating clinical pharmacist capability to schedule appointments, conduct/document ambulatory encounters, and document point-of-care testing results to improve patient-health outcomes.
They also implemented an intricate labeling system throughout the command as part of a Defense Health Agency-led pilot program to support Barcode Medication Administration to improve accurate medication identification and proper documentation for patients in wards and clinics.
The pharmacy became a test site as well for the Navy Pharmacy Management Analytics Program to be successfully incorporated that provided electronic connectivity with patients by being able to send advance text messages and patient-centric information and data to enhance both customer satisfaction and their top priority of patient safety.
“The pharmacy team has adapted and overcome numerous workspace and workflow challenges this year. Their resilience and innovation with respect to the new EHR is leading the way for future roll outs. What our pharmacy team has accomplished this past year is nothing short of phenomenal. We have always known about your exceptional work and dedication to improving our services, and your commitment to our patients. Now those outside the command are also recognizing your achievements and your invaluable contributions to the enterprise as a whole,” said Capt. Jeffrey Bitterman, Naval Hospital Bremerton commanding officer.
Disclaimer: Re-published content may have been edited for length and clarity. Read original post.
DHA assumes management, administration of KMC
Article
10/2/2018

The Keesler Medical Center is the first hospital in the Air Force to transition
Air Force begins transition of hospitals, clinics to the Defense Health Agency
Article
10/2/2018
From a patient perspective, most of these changes should go unnoticed
Robotics key to medical Airmen recruitment, retention, readiness
Article
10/2/2018
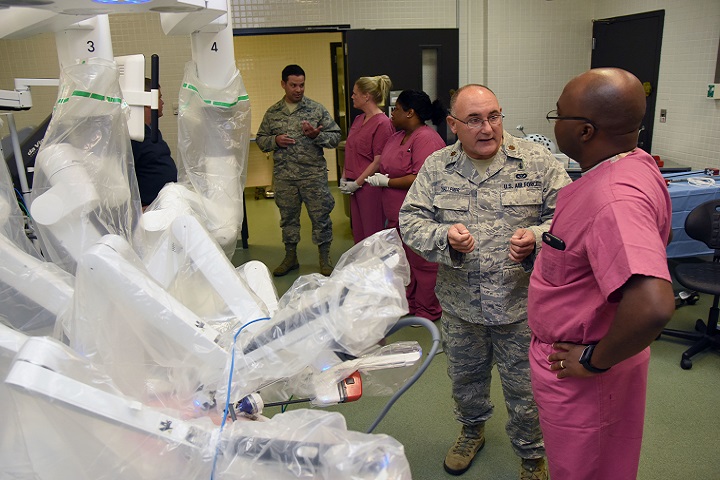
Robotics has been the standard for years in the private sector
Implementing Congressional Direction for Reform of the Military Health System
Policy
Policy Memorandum, signed by Deputy Secretary of Defense Patrick M. Shanahan, to direct implementation of the Military Health System (MHS) organizational reform required by the National Defense Authorization Act.
- Identification #: N/A
- Date: 9/28/2018
- Type: Memorandums
- Topics: Military Hospitals and Clinics
DHA IPM 18-008: Use of Medical Q Services (MQS) Contract by Military Treatment Facilities (MTFs)
Policy
This Defense Health Agency-Interim Procedures Memorandum (DHA-IPM), based on the authority of References (a) through (d): - Instructs MTFs and servicing contracting offices to use the DHA MQS contracts for the procurement of health care staffing requirements for market segments of physician, nurse, dental, and ancillary contract services in the United States and its Territories. - Is effective immediately; it must be incorporated into a forthcoming change to DHA Procedural Instruction 6025.05 (Reference (g)). This DHA-IPM will expire effective 12 months from the date of issue.
- Identification #: 18-008
- Date: 9/19/2018
- Type: DHA Interim Procedures Memorandum
- Topics: Military Hospitals and Clinics
Naval Hospital Jacksonville selected as first Navy facility to transition to DHA
Article
9/13/2018

Naval Hospital Jacksonville’s staff across six locations stands ready to make this a seamless transition for patients
Spine surgery team adds capability, improves readiness
Article
9/11/2018

The benefits of performing complex surgeries in the orthopedic spine clinic go far beyond the operating room
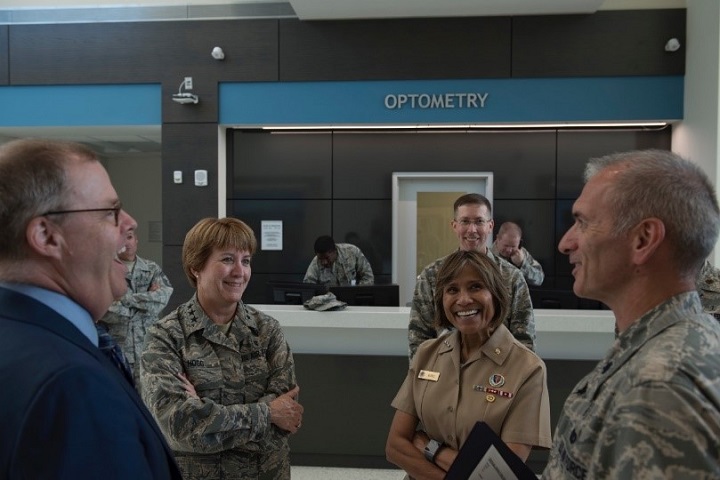
DoD, Air Force medical leaders visit JB Charleston
Article
8/13/2018
By October 2021, all military treatment facilities to include overseas facilities are scheduled to transition to DHA management
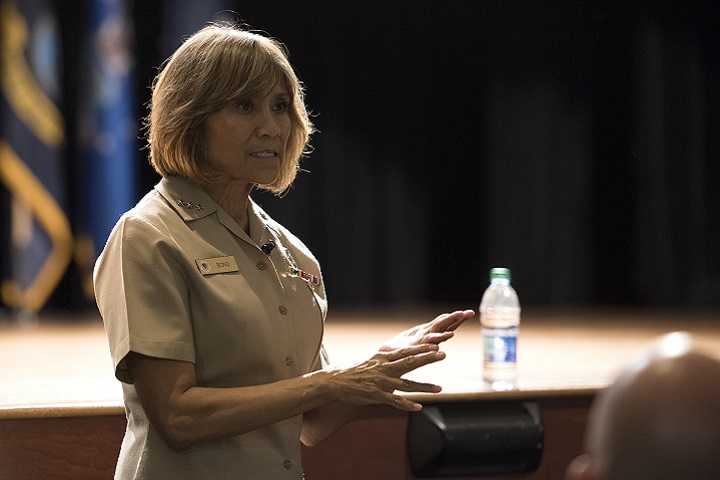
Shanahan discusses medical readiness, DHA transfer at Womack
Article
8/1/2018

The fiscal year 2017 National Defense Authorization Act transfers the administration and management of military medical treatment facilities to the DHA beginning Oct. 1, 2018
NMC Camp Lejeune: 75 years of service expands to civilian community
Article
7/31/2018

Trauma verification helps providers keep skills sharp
Leaders come together to rehearse military healthcare transition
Article
7/31/2018

There should be zero impact on delivery of medical services that support readiness of the force
Two MHS providers achieve top scores in the patient experience survey
Article
6/4/2018

The MHS recently published its annual “Best of the Best” report on medical providers
Project Sea Raven delivers cutting-edge pathogen detection technology
Article
5/31/2018
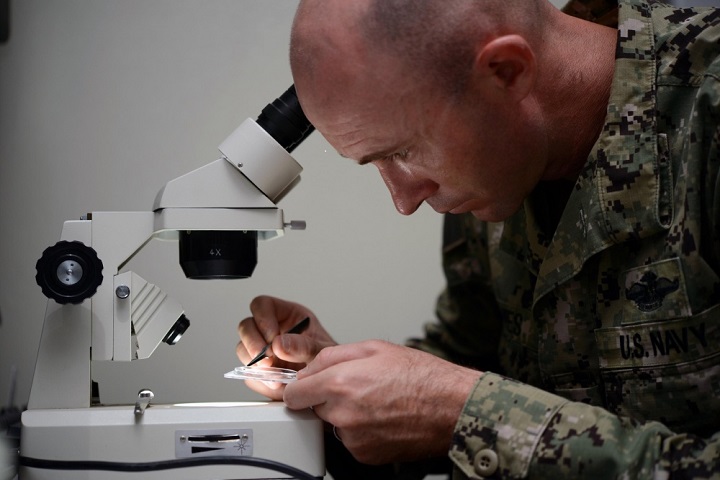
Project Sea Raven is now an integral part of USNS Mercy’s microbiology capacity
The journey to military nursing is different for all
Article
5/9/2018

During National Nurses Week, two Army nurses share insight into their jobs, what motivated them to make a career change, and why they love what they do.
Multinational surgeons participate in first robot-assisted surgery onboard USNS Mercy
Article
5/7/2018

A joint team of multinational surgeons successfully completed a gall bladder removal, using a Da Vinci XI Robot Surgical System





















.png)









No hay comentarios:
Publicar un comentario