
Design Thinking in Health Care
SYSTEMATIC REVIEW — Volume 15 — September 27, 2018
Myra Altman, PhD1,2,3; Terry T.K. Huang, PhD, MPH, MBA4; Jessica Y. Breland, PhD2 (View author affiliations)
Suggested citation for this article: Altman M, Huang TT, Breland JY. Design Thinking in Health Care. Prev Chronic Dis 2018;15:180128. DOI: http://dx.doi.org/10.5888/pcd15.180128.
PEER REVIEWED
Abstract
Introduction
Applying Design Thinking to health care could enhance innovation, efficiency, and effectiveness by increasing focus on patient and provider needs. The objective of this review is to determine how Design Thinking has been used in health care and whether it is effective.
Methods
We searched online databases (PubMed, Medline, Web of Science, CINAHL, and PyscINFO) for articles published through March 31, 2017, using the terms “health,” “health care,” or “healthcare”; and “Design Thinking,” “design science,” “design approach,” “user centered design,” or “human centered design.” Studies were included if they were written in English, were published in a peer-reviewed journal, provided outcome data on a health-related intervention, and used Design Thinking in intervention development, implementation, or both. Data were collected on target users, health conditions, intervention, Design Thinking approach, study design or sample, and health outcomes. Studies were categorized as being successful (all outcomes improved), having mixed success (at least one outcome improved), or being not successful (no outcomes improved).
Results
Twenty-four studies using Design Thinking were included across 19 physical health conditions, 2 mental health conditions, and 3 systems processes. Twelve were successful, 11 reported mixed success, and one was not successful. All 4 studies comparing Design Thinking interventions to traditional interventions showed greater satisfaction, usability, and effectiveness.
Conclusion
Design Thinking is being used in varied health care settings and conditions, although application varies. Design Thinking may result in usable, acceptable, and effective interventions, although there are methodological and quality limitations. More research is needed, including studies to isolate critical components of Design Thinking and compare Design Thinking–based interventions with traditionally developed interventions.
Introduction
Health care systems require continuous innovation to meet the needs of patients and providers (1,2). However, these stakeholders are not always considered when new interventions or system processes are designed, which results in products that remain unused because they do not account for human context, need, or fallibility (3,4). This approach also likely contributes to the decades-long gaps between intervention development and implementation (5). Design Thinking offers a way to close that gap by helping investigators incorporate user needs and feedback throughout the development process.
Design Thinking is an approach that prioritizes developing empathy for users, working in collaborative multidisciplinary teams, and using “action-oriented rapid prototyping” of solutions (2,6). It is an iterative process, with innovation emerging only after cycling through several rounds of ideation, prototyping, and testing, which distinguishes it from the traditional linear and often top-down approach to health intervention design (Figure 1) (1,2,4). Design Thinking has been used across sectors to solve complex problems, including the redesign of an elementary school curriculum to enhance student engagement (7), and in domains such as aviation (8) that, like health care, have high levels of risk. Design Thinking is similar to both “user-centered design” and “human-centered design,” which are both referred to as “Design Thinking” in this article.
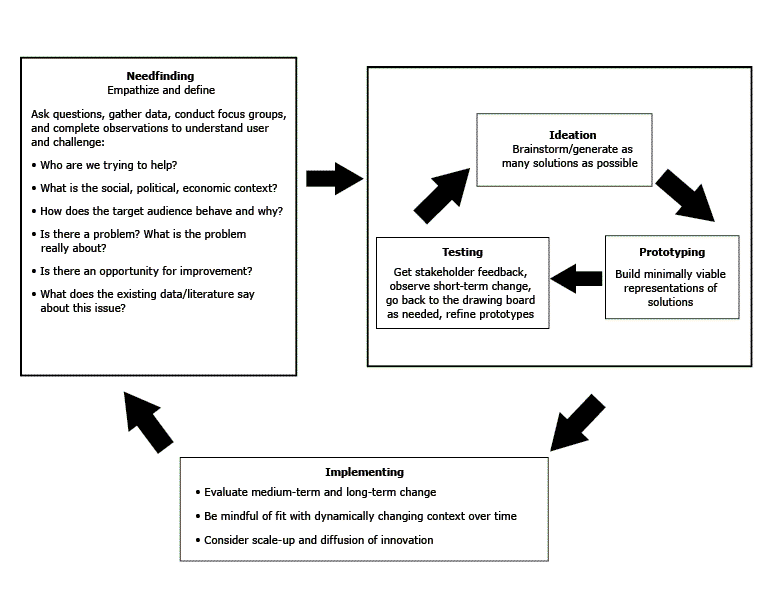
Figure 1.
Design Thinking process, stages of design thinking and examples of exercises used and questions asked in each stage, systematic review on Design Thinking in health care, search results through March 31, 2017. [A text description of this figure is available.]
Design Thinking process, stages of design thinking and examples of exercises used and questions asked in each stage, systematic review on Design Thinking in health care, search results through March 31, 2017. [A text description of this figure is available.]
There is much enthusiasm for the use of Design Thinking in health care, from intervention development to large-scale organizational and systems changes (9). However, health care settings present different challenges than do other domains, so it is important to consider these challenges in assessing whether Design Thinking provides added benefit over traditional approaches. With this in mind, the purpose of this review was to answer the questions, “How has Design Thinking been used to design interventions in health care settings, and have these interventions been effective?”
Methods
Data sources
Studies published through March 31, 2017, were identified through searches of online databases (PubMed, Medline, Web of Science, CINAHL, and PyscINFO) using the following search terms: “health,” “health care,” or “healthcare”; and “Design Thinking,” “design science,” “design approach,” “user centered design,” or “human centered design.” Additional articles were included if they were referenced as original research articles in existing articles. To provide an overview of the range of uses of the Design Thinking approach, we did not limit our review to specific populations or conditions and included articles addressing multiple health promotion and disease prevention topics. Given the search terms, the likely target populations for inclusion were patients and health care professionals and the settings in which they work or seek care.
Study selection
We reviewed selected articles using PRISMA guidelines (10,11) and entered citations into a reference manager, which removed duplicates. To be eligible for inclusion, studies had to be written in English, be published in a peer-reviewed journal, provide outcome data on a health-related intervention, and use Design Thinking in intervention development, implementation or both.
There are multiple definitions of Design Thinking, so we focused on the key principles common to most descriptions of the approach; thus, the list of Design Thinking approaches is not exhaustive. Studies were considered to use Design Thinking if they 1) described user/needs assessment, 2) involved iterative prototyping/testing of the intervention with user feedback, and 3) tested the intervention with target users (2,4). The user/needs assessment could include contextual observation of users in the setting in which they would interact with the innovation, interviews, narrative accounts, and documentation from users, gathering extreme user/outlier stories or a review of existing literature and work (2,6). Prototyping included activities such as creating a series of low-fidelity and high-fidelity prototypes of the potential innovation and refining it multiple times through iterative cycles of feedback from end users, stakeholders, and experts. Testing the intervention with target users included implementing and testing the innovation while continuing to refine it on the basis of user feedback and data (1,2,4). Design Thinking is also similar to other techniques, such as plan-do-study-act cycles and formative evaluations. We considered the emphasis on empathizing with the user and the use of low-fidelity prototyping to be key distinguishing features of Design Thinking, so only articles that explicitly indicate their use of these approaches were included. Initial screening was completed for all selected abstracts, and a second round of screening was completed on eligible full-text articles.
Data abstraction
Data were collected on target users, health conditions, objective of the intervention, details on the Design Thinking process, study design and sample, and reported health outcomes. If information was not reported in the article, we contacted the study authors. Studies were also evaluated to determine whether the intervention improved all targeted outcomes (successful), at least one targeted outcome (mixed success), or no targeted outcomes (not successful). Data quality was assessed using the National Institutes of Health’s (NIH’s) National Heart, Lung, and Blood Institute Study Quality Assessment Tools (12).
Study extraction
Figure 2 presents study flow based on the PRISMA study guidelines (10,11). After the initial search, the authors separately screened all abstracts based on the eligibility criteria. One author reviewed all full-text articles (N = 297), and a second author reviewed roughly 15% as a reliability check. Agreement on inclusion/exclusion was more than 80%. Any abstracts or articles for which there was disagreement or uncertainty were reviewed by 2 authors and discussed until consensus was reached. A total of 26 papers representing 24 interventions were included in the analysis. Two authors reviewed all included studies.
Figure 2.
PRISMA 2009 flow diagram, systematic review on Design Thinking in health care, search results through March 31, 2017. [A text description of this figure is available.]
PRISMA 2009 flow diagram, systematic review on Design Thinking in health care, search results through March 31, 2017. [A text description of this figure is available.]
Results
Study characteristics
A summary of all included studies is provided in (Table 1). Eleven studies were successful (13–25), 12 reported mixed success (26–37), and one reported no success (38) (Table 1 and Table 2). Sample sizes of included studies ranged from 12 to 291, but most studies were small; 14 studies had fewer than 40 participants. Eleven (45.8%) used a control group (15,17,18,24,26–29,31,33,35,38,42), and 4 (16.6%) compared a design-thinking intervention to an intervention designed using traditional methods (17,18,24,26,35). Two of the studies included were “good” quality, 13 were “fair” quality, and 9 were “poor” quality. All studies used Design Thinking methodology in intervention development, and 3 also used it for implementation (16,20,25,43)
The 24 included interventions targeted a range of conditions, including 19 related to physical health (17 unique conditions), 2 related to mental health, and 3 related to systems processes. Approximately two-thirds of the interventions were mobile telephone–based or tablet-based.
Summary of findings by target user
Patient-facing interventions (n = 11). Five interventions were successful: 4 with a pre/post design (13,19,22,23,44) and 1 pilot randomized control trial (RCT) (15). Five reported mixed success, including one pre/post design (31), one pilot RCT (29), one RCT (28), one cohort study (47), and one unblinded, randomized crossover design (33). One, a pilot RCT, was not successful (46).
Provider-facing interventions (n = 9). Six were successful, including 3 studies using a pre/post design (16,20,25), one field experiment (14), one using a quasi-experimental crossover design (24), and one cross-sectional study (21). Three had mixed success, including 2 studies with an experimental crossover design (17,18,26) and one with primarily a pre/post design, one portion of which was a randomized crossover design (35).
Patient-facing and provider-facing interventions (n = 2). Both reported mixed success and were pre/post designs (30,34,45).
Caregiver-facing or family-facing interventions (n = 2). Both reported mixed success, one in a pilot RCT (27,39) and one using a pre/post design (32).
Summary of Randomized-Controlled Trials (K = 5). Of the RCTs and pilot RCTs reviewed, one demonstrated success on all outcomes (15,40), 3 showed mixed success (27–29,39,41), and one reported no enduring significant results (38,46).
Summary of studies directly testing Design Thinking methodology
Four studies directly compared interventions created with Design Thinking to interventions created with traditional methods. In one study with a within-sample experimental crossover design (26), a Design Thinking–based graphical information display to improve nurses’ ability to detect changes in patients’ physiological states in an intensive care unit (ICU) was compared with a conventional display in commercial, electronic ICU charting systems. The Design Thinking intervention resulted in improved detection of changes in patient states and greater ease of use, usefulness, satisfaction, and support of understanding, but no differences in workload for nurses (26). Another study using an experimental crossover design compared 2 computer interfaces designed to display drug interaction alerts, one developed using Design Thinking and one using traditional software (17,18). Whereas the design of the traditional software was not described, the traditional display included only basic text information. In this study, users (ICU nurses) were more efficient and effective, and reported higher satisfaction with the Design Thinking interface. Another study using a quasi-experimental crossover design used Design Thinking to develop an application to guide clinicians in detecting and scoring the severity of graft versus host disease (GvHD) (24). When compared with paper-based NIH guidelines, users of the application (app) signficantly improved diagnostic and scoring accuracy. A final study compared a Design Thinking–based app that provided nurses with information about antibiotic use with regular information sources (which were not described) (35). In the randomized portion of this study, nurses using the app found information on antibiotic use more quickly; however, the app did not enhance their ability to improve antibiotic-related behaviors. (Only 7 participants were included in the randomized portion of the study.) Whereas the development of the control intervention was not fully described in these papers, based on the limited descriptions given, it is likely that it did not include key elements of Design Thinking such as user feedback and prototyping.
Discussion
The 24 interventions summarized in this review provide an overview of the breadth of Design Thinking’s applicability in health care and demonstrate that it is feasible and applicable to multiple health care domains. It has been applied across a range of diverse patient populations and conditions, including chronic obstructive pulmonary disease (28,34), diabetes (34,47), caregiver stress (27), and posttraumatic stress disorder (22). It also has been applied to systems process changes, such as nursing handoffs (16) and drug–drug interaction alerts (17,18). Results also demonstrate that, although it is often applied to electronic interventions, Design Thinking is feasible for use in other modalities (eg, on paper, in person).
Initial results of the interventions included in this review are promising; all but one demonstrated positive effects on at least one identified outcome, and half showed positive effects on all measured outcomes. In addition, in the studies that directly compared the Design Thinking intervention with a traditional intervention, the Design Thinking intervention generally demonstrated improved outcomes and higher usability and satisfaction.
However, none of these studies were RCTs with large sample sizes. Design Thinking interventions have been tested primarily in pre/post designs or pilot RCTs with small samples. Furthermore, most studies included were poor or fair quality, with only 2 being considered good quality. Importantly, the criteria used to assess quality were based on traditional research approaches, and many of the features of poor-quality studies were included by design; some had small sample sizes to generate insights and to test assumptions rapidly, and some were pilot studies. This feature of Design Thinking also may account for the limited use of large RCTs; however, this poses a challenge when evaluating the effectiveness of the approach. More work in this area using more rigorous methods and larger samples is critical to fully understanding the benefits of Design Thinking. Although many studies that used Design Thinking were excluded from our review because they did not include sufficient outcome data (n = 131), full-scale trials of many of these interventions are under way, results of which will provide more evidence about the effectiveness of this approach in health care. In addition, no studies measured Design Thinking directly to explain how or what components of Design Thinking lead to improved usability and effectiveness, limiting the field’s ability to disseminate the most effective components and refine the Design Thinking approach for health care.
Design Thinking methods varied among the studies reviewed. For example, only 6 studies conducted contextual observations of users during the needs assessment phase, no studies reported a brainstorming stage, 10 studies did not use low-fidelity prototypes, and some reported a small number of iterations (eg, one mixed-success trial had 4 intervention iterations, but only 2 iterations were evaluated with target users [27]). Using more thorough and structured Design Thinking methodology may have resulted in more consistent and enhanced outcomes. At the same time, Design Thinking is meant to be flexibly applied. Future work should balance that flexibility with the potential benefits of a more systematic approach.
Our results suggest that one area where Design Thinking could be especially useful is in designing interventions for underserved populations whose needs may be overlooked by other approaches. For example, the study of a mobile health tool for detecting and managing cardiovascular disease in rural India required significant feedback from the end users — minimally trained health workers — to ensure that the intervention was suited to their level of technological familiarity as well as the inconsistent technical infrastructure (eg, creating a one-touch navigation system) (21). Using Design Thinking allowed the multidisciplinary team to question assumptions and biases and develop an intervention that was successful, acceptable, and feasible to the actual users, an outcome that may not have been possible using traditional methods (21). Another study evaluated the impact of an education tool to enhance long-acting contraceptive use in a clinic serving mostly African American patients who were included early in the usability testing process to ensure the tool met their needs. Several changes were made as a result, such as including more peer testimonials, which likely increased the tool’s impact and relevance (29). In this way, Design Thinking could also pair well with other approaches that prioritize the inclusion of users in service of reducing health disparities, such as community-based participatory research (48).
Tensions when using Design Thinking in health care
In their text and through our analysis, the studies included in this review show several challenges to consider when applying Design Thinking to health care. First, there is the possibility of tension between what users want and what providers and researchers believe to be beneficial based on research and expertise (49). Whereas in industry, where an innovation designer may prioritize customers’ preferences to maximize profits, in health care a balance must be struck between creating interventions that are effective and sufficiently palatable and feasible so that they will be used by providers and patients.
Second, tension may exist between the needs assessment, a fundamental step of Design Thinking, and existing literature and evidence base for some conditions. That is, given the evidence, intervention developers may not be willing or see it necessary to conduct their own needs assessment using observation or interview strategies or to brainstorm creative solutions. Indeed, 7 of the studies included in this review reported literature reviews, and possibly expert consultation, as their only needs assessment steps, and none reported brainstorming. One way to overcome this tension is to view evidence as a set of design constraints in which needs assessment, brainstorming, ideation, and prototyping should occur.
A third possible tension relates to balancing the Design Thinking approach of understanding the narrative of outliers with traditional health research methods that prioritize statistics on large samples to produce generalizable results. Conclusions drawn from small user samples should be tested in broader populations to ensure their applicability. Mixed-methods approaches that use both strategies may reduce this tension. For example, a research team that uses a qualitative Design Thinking approach early in the research process (eg, user observations, focus groups, and usability tests with small groups of target users) may be able to generate insights into the key needs of the target population. This approach may also find ways to address these needs, and subsequent quantitative testing of the developed interventions in broader samples will allow the group to evaluate whether their assumptions generalize to the broader population, and the intervention will be more effective as a result.
Fourth, there is inherent tension between a central philosophy of the prototyping process in Design Thinking — to rapidly move through low-fidelity then high-fidelity iterations to fail early and often to more quickly reach a better design (50) — and the risk of serious negative outcomes due to health care failures (eg, death). Many of the studies did not use low-fidelity prototyping or multiple rapid iterations, perhaps because of this tension. However, although there may be some reluctance to experiment with low-fidelity prototypes in health care where morbidity and mortality are at stake, there are low-stakes approaches to low-fidelity prototyping that may minimize risk and improve the pace of innovation (eg, storyboards to illustrate a new clinic process).
Intervention development and implementation: case example
Considering the role of Design Thinking is important, not only in efficacious intervention development but also in effective implementation into practice (5). Only 3 of the included interventions addressed implementation, but this limited implementation provides insights. For example, in designing a new process for facilitating nurse handoffs between shifts, Lin and colleagues conducted an extensive 6-month intervention development design process that was user-focused and empathic and had rapid iteration in pilot sites (43). However, despite this strong preliminary work, the intervention was not readily accepted when implemented in other clinics. As a participant stated:
After the concepts had been co-developed and field tested with our pilot units . . . we assumed the units were “bought in” to the idea of the change. . . . Surprisingly, our approach to the training resulted in criticism and created skepticism [at other clinics]. . . . They attributed this to “not made here” sentiments from those units not involved in the original design.
To overcome this tension, the team involved additional stakeholders to develop a more user-centered process for the implementation of their Design Thinking innovation, after which they successfully implemented the innovation across 125 nursing units in 14 hospitals over 2 years (16). This study highlights the importance of understanding the context of the setting and users, both when developing and implementing an intervention using a Design Thinking approach. It should also be noted that this process required significant time and energy from stakeholders. One stakeholder commented, “Don’t get me wrong. What we did was fantastic. But it took a lot out of us” (43). This study highlights the importance of staying true to the user-centered nature of Design Thinking throughout the process — from development to implementation — to maximize implementation success. It also highlights the challenges in using this approach. Teams using Design Thinking should be prepared for a more intensive process than traditional, less iterative and user-centered methods.
Limitations
Given the varied outcomes included in the review and the inconsistent reporting of qualitative outcomes it was difficult to make comparisons across studies. The range of study types and limited number of large scale RCTs testing intervention effects also made it difficult to draw definitive conclusions about effectiveness. At the same time, given that there was only one study with a null result, there was likely publication bias, which may have led to overestimation of the effectiveness of Design Thinking. It is also possible that investigators used methods but did not report them (eg, prototyping). In addition, we did not assess the use of Design Thinking in other health care areas where it may be beneficial, such as the design of physical spaces. Finally, Design Thinking–based health care innovations that were developed and implemented outside research contexts may exist and are thus not reported in the literature.
Conclusions
Design Thinking is being used in varied health care settings and health conditions, and more studies are forthcoming. This review suggests that Design Thinking may result in more usable, acceptable, and effective interventions compared with traditional expert-driven methods. However, there is inconsistent use of the methodology and significant limitations inherent in the studies, which limits our ability to draw conclusions about this approach. Future studies may benefit from focusing on comparing interventions developed using Design Thinking methods with traditionally developed interventions, including those with RCT designs, and identifying the most useful components of Design Thinking methods.
Overall, Design Thinking is a promising approach to intervention development, implementation, and dissemination that may increase the acceptability and effectiveness of health care interventions by actively engaging patients and providers in the design process and rapidly iterating innovation prototypes to maximize success.
Acknowledgments
The research was supported by the Department of Veterans Affairs (VA), Veterans Health Administration, Health Services Research and Development Service (HSR&D). Dr Breland is a VA HSR&D Career Development awardee at the VA Palo Alto (15-257). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. There is no copyrighted material used in this article, and no copyrighted surveys, instruments, or tools were used in this article.
The authors thank Ms Elon Hailu for her help editing the manuscript. At the time of the research, Dr Altman was affiliated with the Department of Psychology, Washington University in St. Louis, St. Louis, Missouri, and the VA Palo Alto Health Care System, Menlo Park, California.
Author Information
Corresponding Author: Myra Altman, PhD, Postdoctoral Design Fellow, Clinical Excellence Research Center, Stanford University, 75 Alta Rd, Stanford, CA 94305. Telephone: 603-306-6231. Email: myra.altman@gmail.com.
Author Affiliations: 1Washington University in St. Louis, St. Louis, Missouri. 2VA Palo Alto Health Care System, Menlo Park, California. 3Stanford University, Stanford, California. 4Center for Systems and Community Design, Graduate School of Public Health and Health Policy, City University of New York, New York, New York.
References
- MacFadyen JS. Design thinking. Holist Nurs Pract 2014;28(1):3–5. CrossRef PubMed
- Roberts JP, Fisher TR, Trowbridge MJ, Bent C. A design thinking framework for healthcare management and innovation. Healthc (Amst) 2016;4(1):11–4. CrossRef PubMed
- Searl MM, Borgi L, Chemali Z. It is time to talk about people: a human-centered healthcare system. Health Res Policy Syst 2010;8(1):35. CrossRef PubMed
- Lyon AR, Koerner K. User-centered design for psychosocial intervention development and implementation. Clin Psychol (New York) 2016;23(2):180–200. CrossRef PubMed
- Munro CL, Savel RH. Narrowing the 17-year research to practice gap. Am J Crit Care 2016;25(3):194–6. CrossRef PubMed
- Ferreira FK, Song EH, Gomes H, Garcia EB, Ferreira LM. New mindset in scientific method in the health field: Design Thinking. Clinics (Sao Paulo) 2015;70(12):770–2. CrossRef PubMed
- Kelley D, Kelley T. Creative confidence: unleashing the creative potential within us all. Danvers (MA): Crown Publications; 2013.
- Hall A, Mayer T, Wuggetzer I, Childs PRN. Future aircraft cabins and design thinking: optimisation vs. win-win scenarios. Propulsion and Power Research 2013;2(2):85–95. CrossRef
- Bevan H, Robert G, Bate P, Maher L, Wells J. Using a design approach to assist large-scale organizational change: “10 High Impact Changes” to improve the National Health Service in England. J Appl Behav Sci 2007;43(1):135–52. CrossRef
- Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G, et al. ; PRISMA-IPD Development Group. Preferred reporting items for a systematic review and meta-analysis of individual participant data: The prisma-ipd statement. JAMA 2015;313(16):1657–65. CrossRef PubMed
- Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6(7):e1000097. CrossRef PubMed
- National Institutes of Health, National Heart Lung, and Blood Institute. Study quality assessment tools. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed May 4, 2018.
- Adirim T, Chafranskaia A, Nyhof-Young J. Investigating the impact of socioeconomic status on the effectiveness of a pamphlet on achieving and maintaining bone health in breast cancer survivors: a patient education resource development primer. J Cancer Educ 2012;27(1):54–8. CrossRef PubMed
- Kuipers DA, Wartena BO, Dijkstra BH, Terlouw G, van T Veer JT, van Dijk HW, et al. iLift: A health behavior change support system for lifting and transfer techniques to prevent lower-back injuries in healthcare. Int J Med Inform 2016;96:11–23. CrossRef PubMed
- DeVito Dabbs A, Dew MA, Myers B, Begey A, Hawkins R, Ren D, et al. Evaluation of a hand-held, computer-based intervention to promote early self-care behaviors after lung transplant. Clin Transplant 2009;23(4):537–45. CrossRef PubMed
- Lin M, Heisler S, Fahey L, McGinnis J, Whiffen TL. Nurse knowledge exchange plus: human-centered implementation for spread and sustainability. Jt Comm J Qual Patient Saf 2015;41(7):303–12. CrossRef PubMed
- Luna D, Otero C, Risk M, Stanziola E, González Bernaldo de Quirós F. impact of participatory Design for Drug-Drug Interaction Alerts. A comparison study between two interfaces. Stud Health Technol Inform 2016;228:68–72. PubMed
- Luna DR, Rizzato Lede DA, Otero CM, Risk MR, González Bernaldo de Quirós F. User-centered design improves the usability of drug-drug interaction alerts: Experimental comparison of interfaces. J Biomed Inform 2017;66:204–13. CrossRef PubMed
- McGaffey A, Hughes K, Fidler SK, D’Amico FJ, Stalter MN. Can Elvis Pretzley and the Fitwits improve knowledge of obesity, nutrition, exercise, and portions in fifth graders? Int J Obes 2010;34(7):1134–42. CrossRef PubMed
- Pottenger BC, Davis RO, Miller J, Allen L, Sawyer M, Pronovost PJ. Comprehensive Unit-based Safety Program (CUSP) to Improve Patient Experience: how a hospital enhanced care transitions and discharge processes. quality management in health care 2016;25(4):197-202.
- Raghu A, Praveen D, Peiris D, Tarassenko L, Clifford G. Engineering a mobile health tool for resource-poor settings to assess and manage cardiovascular disease risk: SMARThealth study. BMC Med Inform Decis Mak 2015;15(1):36. CrossRef PubMed
- Rizzo A, Difede J, Rothbaum BO, et al. Development and early evaluation of the Virtual Iraq/Afghanistan exposure therapy system for combat-related PTSD. In: Barchas JD, Difede J, editors. Psychiatric and Neurologic Aspects of War. Vol. 1208. Hoboken (NJ): John Wiley and Sons; 2010. p. 114–25.
- Sánchez-Morillo D, Crespo M, León A, Crespo Foix LF. A novel multimodal tool for telemonitoring patients with COPD. Inform Health Soc Care 2015;40(1):1–22. CrossRef PubMed
- Schoemans H, Goris K, Durm RV, Vanhoof J, Wolff D, Greinix H, et al. Development, preliminary usability and accuracy testing of the EBMT ‘eGVHD App’ to support GvHD assessment according to NIH criteria-a proof of concept. Bone Marrow Transplant 2016;51(8):1062–5. CrossRef PubMed
- Trail-Mahan T, Heisler S, Katica M. Quality improvement project to improve patient satisfaction with pain management using human-centered design. J Nurs Care Qual 2016;31(2):105–12, quiz 113–4. CrossRef PubMed
- Anders S, Albert R, Miller A, Weinger MB, Doig AK, Behrens M, et al. Evaluation of an integrated graphical display to promote acute change detection in ICU patients. Int J Med Inform 2012;81(12):842–51. CrossRef PubMed
- Cristancho-Lacroix V, Moulin F, Wrobel J, Batrancourt B, Plichart M, De Rotrou J, et al. A web-based program for informal caregivers of persons with Alzheimer’s disease: an iterative user-centered design. JMIR Res Protoc 2014;3(3):e46–46. CrossRef PubMed
- Farmer A, Williams V, Velardo C, Shah SA, Yu LM, Rutter H, et al. Self-management support using a digital health system compared with usual care for chronic obstructive pulmonary disease: randomized controlled trial. J Med Internet Res 2017;19(5):e144. CrossRef PubMed
- Gilliam ML, Martins SL, Bartlett E, Mistretta SQ, Holl JL. Development and testing of an iOS waiting room “app” for contraceptive counseling in a Title X family planning clinic. Am J Obstet Gynecol 2014;211(5):481.e1–8. CrossRef PubMed
- Hartzler AL, Izard JP, Dalkin BL, Mikles SP, Gore JL. Design and feasibility of integrating personalized PRO dashboards into prostate cancer care. J Am Med Inform Assoc 2016;23(1):38–47. CrossRef PubMed
- Kamal N, Fels S, Fergusson M. Online social networks for health behaviour change: designing to increase socialization. Comput Human Behav 2014;41:444–53. CrossRef
- Koehly LM, Morris BA, Skapinsky K, Goergen A, Ludden A. Evaluation of the Families SHARE workbook: an educational tool outlining disease risk and healthy guidelines to reduce risk of heart disease, diabetes, breast cancer and colorectal cancer. BMC Public Health 2015;15(1):1120. CrossRef PubMed
- van Besouw RM, Oliver BR, Grasmeder ML, Hodkinson S, Solheim H. Evaluation of an interactive music awareness program for cochlear implant recipients. Music Percept 2016;33(4):493–508. CrossRef
- Verwey R, van der Weegen S, Spreeuwenberg M, Tange H, van der Weijden T, de Witte L. Technology combined with a counseling protocol to stimulate physical activity of chronically ill patients in primary care. Stud Health Technol Inform 2014;201:264–70. PubMed
- Wentzel J, van Drie-Pierik R, Nijdam L, Geesing J, Sanderman R, van Gemert-Pijnen JE. Antibiotic information application offers nurses quick support. Am J Infect Control 2016;44(6):677–84. CrossRef PubMed
- Yu CH, Parsons JA, Mamdani M, Lebovic G, Hall S, Newton D, et al. A web-based intervention to support self-management of patients with type 2 diabetes mellitus: effect on self-efficacy, self-care and diabetes distress. BMC Med Inform Decis Mak 2014;14(1):117. CrossRef PubMed
- Wachter SB, Agutter J, Syroid N, Drews F, Weinger MB, Westenskow D. The employment of an iterative design process to develop a pulmonary graphical display. J Am Med Inform Assoc 2003;10(4):363–72. CrossRef PubMed
- Welch JL, Astroth KS, Perkins SM, Johnson CS, Connelly K, Siek KA, et al. Using a mobile application to self-monitor diet and fluid intake among adults receiving hemodialysis. Res Nurs Health 2013;36(3):284–98. CrossRef PubMed
- Cristancho-Lacroix V, Wrobel J, Cantegreil-Kallen I, Dub T, Rouquette A, Rigaud A-S. A web-based psychoeducational program for informal caregivers of patients with Alzheimer’s disease: a pilot randomized controlled trial. J Med Internet Res 2015;17(5):e117. CrossRef PubMed
- DeVito Dabbs A, Myers B, McCurry K. User-centered design and the development of interactive health communication applications. Comput Nurs 2009;27(3):175.
- Velardo C, Shah SA, Gibson O, Clifford G, Heneghan C, Rutter H, et al. ; EDGE COPD Team. Digital health system for personalised COPD long-term management. BMC Med Inform Decis Mak 2017;17(1):19. CrossRef PubMed
- Kamal N, Fels S, Blackstock M, Ho K. VivoSpace: towards health behavior change using social gaming. Paper presented at: Entertainment Computing — ICEC 2011. Berlin, Germany, and Heidelberg, Germany; 2011.
- Lin MC, Hughes BL, Katica MK, Dining-Zuber C, Plsek PE. Service design and change of systems: human-centered approaches to implementing and spreading service design. Int J Des 2011;5(2):73–86.
- McLay RN, Graap K, Spira J, Perlman K, Johnston S, Rothbaum BO, et al. Development and testing of virtual reality exposure therapy for post-traumatic stress disorder in active duty service members who served in Iraq and Afghanistan. Mil Med 2012;177(6):635–42. CrossRef PubMed
- van der Weegen S, Verwey R, Spreeuwenberg M, Tange H, van der Weijden T, de Witte L. The development of a mobile monitoring and feedback tool to stimulate physical activity of people with a chronic disease in primary care: a user-centered design. JMIR Mhealth Uhealth 2013;1(2):e8. CrossRef PubMed
- Welch JL, Siek KA, Connelly KH, Astroth KS, McManus MS, Scott L, et al. Merging health literacy with computer technology: self-managing diet and fluid intake among adult hemodialysis patients. Patient Educ Couns 2010;79(2):192–8. CrossRef PubMed
- Yu CH, Parsons JA, Hall S, Newton D, Jovicic A, Lottridge D, et al. User-centered design of a web-based self-management site for individuals with type 2 diabetes – providing a sense of control and community. BMC Med Inform Decis Mak 2014;14(1):60. CrossRef PubMed
- Henderson VA, Barr KL, An LC, Guajardo C, Newhouse W, Mase R, et al. Community-based participatory research and user-centered design in a diabetes medication information and decision tool. Prog Community Health Partnersh 2013;7(2):171–84. CrossRef PubMed
- Witteman HO, Dansokho SC, Colquhoun H, Coulter A, Dugas M, Fagerlin A, et al. User-centered design and the development of patient decision aids: protocol for a systematic review. Syst Rev 2015;4(1):11. CrossRef PubMed
- Thoring K. M RM, #252, ller. Understanding the creative mechanisms of design thinking: an evolutionary approach. Procedings of the Second Conference on Creativity and Innovation in Design. Eindhoven, Netherlands; 2011.





















.png)









No hay comentarios:
Publicar un comentario