
Surgeons share secrets of residency success

Surgeons in the operating room at Madigan Army Medical Center. (U.S. Army photo by John Wayne Liston)
JOINT BASE LEWIS-MCCHORD, Wash. – Over the last 15 years, residents graduating from Madigan Army Medical Center's general surgery residency program have passed the exam for board certification on their first attempt at a nation-topping rate of 97.6 percent.
The American Journal of Surgery recently published a long-term study that ranks 231 general surgery residency programs across the country by this measure. By nearly two percentage points over the next ranked program, Madigan's residents taking exam over the 15-year duration of the study put the program in the number one spot. The pass rate that Madigan scored is well above the mean of 72.9 percent.
To become a board-certified general surgeon, passing a combination of a computerized multiple choice qualifying exam and an oral certifying exam is required.
Because of its value in the surgical field, this pass rate is seen as a significant measure of the success of a residency program. The study makes the overall success of military programs in achieving board certification apparent.
"I think we attract a special breed of residents," said Army Lt. Col. (Dr.) Vance Sohn, the residency program director and chief of general surgery. "That's the type of person that we recruit and retain — the people who don't shy away from challenges. We want to be in the action," he added.
Of the 231 programs evaluated, eight were military, with six of those being Army. All of the military programs were ranked in the top half. Five of the six Army residencies were in the top third and two scored in the top three. Brooke Army Medical Center at Fort Sam Houston, Texas, occupies the third spot on the list.
Selecting Character and Promise
"The article divides it into military programs, academic programs, and civilian programs. The military programs were statistically better overall than any of the other two. And I think it has a lot to do with our selection process. They signed up for a military career and all the trappings that go with that — the responsibilities and things. You're getting a different level of committed individual. That's part of it," explained Dr. Joseph Homann, a surgeon and key member of the faculty.
Sheer numbers also allow Madigan to be choosy when selecting its residents.
"You have more people that want to do general surgery than the Army has places to train people so you really get the best of the best," agreed Army Capt. (Dr.) Michael Lallemand, a chief resident currently in his sixth year in the program.
"If you get an 89 percentile in the nation, you're in the bottom quarter of Madigan in our annual in-training exam. That's unheard of in any program. In any other program, you get an 89 percentile in the nation, you are doing very well," Sohn said.
More than simply the supply and demand aspect is the vast difference between the selection process within the military and the civilian side.
As civilians apply to 1 of the 200+ programs, they submit their transcripts and possibly spend a day visiting a facility. That's the extent of visibility either candidate or faculty gets in determining whether the fit is right or not for the next five to six years.
In the military, a medical student does a full four-week rotation working within their prospective program. That makes the selection process much more informed, on both sides. The resident gets to interact with the faculty and staff within the program who, in turn, get to see the candidate in action.
"You get to work with them professionally. See how they work in clinic, see how they work on the wards," said Lallemand. "You get that time to figure out — do we think this person is going to be successful or not," he said.
The military programs seem to have an advantage from the start. But, Madigan stands out even beyond that. A number of possible reasons come to the fore.
The Madigan Approach
When he attends meetings and conferences off base, Sohn gets asked the same question again and again. "'What is it that you guys do that makes you so different?' We don't have a separate book that only we study out of," he said.
Yet, there are things that are unique to Madigan's way of training general surgeons.
Every Thursday is dedicated to training. Every single one. There is also a full year dedicated to research. That is now common Army-wide, but wasn't when Madigan started doing it. It is not common in the typical civilian residency program.
Residents here also get some good preparation for that oral exam. As they work on-call in their second and third years, they are required to present in a morning conference on all their patients and activities. Then, during their last three years of residency, they work with a hospital in Seattle to do rounds of mock oral exams twice a year.
Being able to answer the questions of what to do in the oral exam situation is vital, but developing the surgical skills to perform in the operating room is clearly paramount.
"I think one of the big advantages to our program, especially compared to some of the civilian programs," commented Lallemand, "is that literally day one of intern year, the interns were in the operating room."
He noted that those initial procedures are minor things like draining an abscess, and are accompanied by intensive, over-the-shoulder supervision by faculty. Jumping right in and getting comfortable in the operating room is important, though.
"That's not necessarily the experience interns get everywhere in the country. That's one of the big strengths of our program is you get in the operating room right away and you get that experience."
As focused as faculty is on perpetuating the areas of strength in the program, they are also addressing weaknesses.
"Each year there are little incremental changes. We have discussions and we identify areas that are perhaps a little weak," said Homann.
Lallemand points to one area that has some room for improvement. "Anyone who's being honest isn't going to look at our program and say there's a lot of diversity. I think that's a weakness of our program," he said. In specific reference to the number of women in the program, he noted that, "the demographics are changing." The program has heard this concern from medical students doing their rotation and has added female faculty.
Stability and Sustainment
A number of the faculty, both current and throughout the study's length, did their residency here to include Sohn and Army Lt. Col. (Dr.) Matt Eckert, the trauma medical director and associate residency program director.
In addition to long-term dedication to the program by active duty surgeons, there is a contingent of former Madigan colonels who now work as civilian faculty.
"I came here in 2004 when most of the active duty people were deployed and they just needed help from people who were used to the system. That's 15 years ago. That covers the spectrum of this report," said Homann.
"I think having a stable staff really helps with the educational process," Homann said. Madigan was his last duty station before retiring from active duty.
"We've had a long-standing focus and intentional development of the faculty and the residency because we had a program that worked and we wanted to stick with it. That's a little unique in the military because typically even among surgical residencies in the military there's still a lot of movement among staff," said Eckert.
The Mission at Hand
"I really try to impress upon them what the mission for our training is," said Sohn. "We have a very defined role in that we are going to deploy to the most remote and austere environments. We're going to be given the least amount of resources and we're going to say, 'you have to succeed,'" he added.
Having been deployed numerous times himself, Sohn knows the skills and knowledge his residents will need in that situation. He works to nurture a drive in them.
"It's a long six years and they work very, very hard for six years. Our bar, our standards are very high because again, it's not something artificial; they will deploy," he said.
Lallemand, though he has not yet deployed, has clearly taken this mission awareness to heart.
"It's a very real possibility that six years from now when you're just finishing your residency and I've been out for six years and we deploy together and, you know, some Soldier's life depends on how well we can perform that day. To be able to perform your best, I have to rely on you to have gotten everything you can out of your residency," he said.
Culture of Excellence
Ultimately, the aspect faculty and residents bring forward as a key factor in the success of the program is that high-potential residents come into a program that is accustomed to success and, therefore, has very high expectations for them.
"We have a hard-wired culture of excellence here and I think that's really what sustains us," said Sohn.
High expectations exist for residents from the start of their first, or intern, year and they merely build from there.
Lallemand finds the expectation both intimidating and inspiring. By the final, or chief resident, year they are part of the mechanism that insists the bar is met.
"You have a team of medical students and residents looking up to you now. You have to be able to lead your people and get your people to want to be better for you because the people that were ahead of you made you better," said Lallemand. "You're always expected to be a teacher."
The staff and chief residents push until a resident doesn't know an answer. "Then, when you don't know the answer, that's where the opportunity to learn comes from. If you don't get to the point where you don't know something every day, I kind of get the sense that the faculty and the senior residents have failed the junior residents because we haven't taught them anything," said Lallemand.
Lallemand makes clear that all this pushing is borne of a passion for the craft, the program and those within it. "The faculty really care," he said.
"Being a surgeon is one of the greatest jobs in the world," concluded Homann. "And it's still fun, especially," he noted, "seeing the young people come along."
Disclaimer: Re-published content may have been edited for length and clarity. Read original post.
Fleet surgical team saves life aboard USS Somerset
Article
12/6/2018

We were able to determine he had acute appendicitis
USNS Comfort conducts mass casualty training exercise
Article
10/15/2018

A mass casualty event, by nature, is chaotic
DHA IPM 18-012: The DoD Medical Ethics Program (DoDMEP) in the Military Health System (MHS)
Policy
This Defense Health Agency-Interim Procedures Memorandum (DHA-IPM), based on the authority of References (a) through (c), and in accordance with the guidance of References (d) through (k), establishes Defense Health Agency’s (DHA) procedures that: • Apply to Active Duty Service members, namely Active Component members and Reserve Component members on active duty for a period of more than 30 days, who, hereafter, are referred to collectively as Active Duty Service members (References (e) and (f)). • Establish a set of common guidelines, standards, and procedures governing the DoDMEP for military health care personnel in all locations. • Outline implementing procedures for DHA collaboration with the DoDMEP office, to be known as the DoD Medical Ethics Center (DMEC), which is to operate under the direction of the President of the Uniformed Services University of the Health Sciences (USUHS). • Implement guidance for the DoD mission, vision, guiding principles of the DoDMEP (DMEC) as set forth in Reference (g) and delineate areas of responsibility between the DHA and USUHS, including: o The provision of medical ethics education and training (E&T) to health care providers and other health care personnel; o Creation and maintenance of a DMEC portal; and o Medical ethics consultation services to MHS health care personnel across all settings. • This DHA-IPM is effective immediately and will expire effective 12 months from the date of issue.
- Identification #: 18-012
- Date: 10/9/2018
- Type: DHA Interim Procedures Memorandum
- Topics: Access, Cost, Quality, and Safety
A 'Pharmacy Phamily' team effort recognized at Naval Hospital Bremerton
Article
10/3/2018

Naval Hospital Bremerton’s pharmacy selected for the 2018 Navy Pharmacy Team Award
Robotics key to medical Airmen recruitment, retention, readiness
Article
10/2/2018
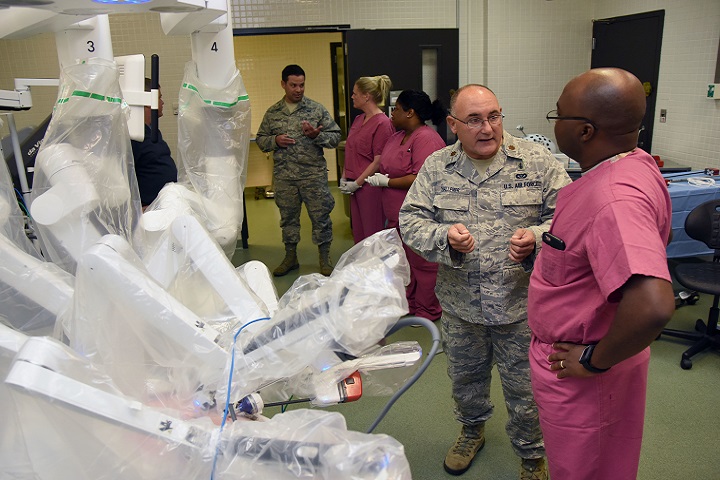
Robotics has been the standard for years in the private sector
DHA assumes management, administration of KMC
Article
10/2/2018

The Keesler Medical Center is the first hospital in the Air Force to transition
Air Force begins transition of hospitals, clinics to the Defense Health Agency
Article
10/2/2018
From a patient perspective, most of these changes should go unnoticed
Implementing Congressional Direction for Reform of the Military Health System
Policy
Policy Memorandum, signed by Deputy Secretary of Defense Patrick M. Shanahan, to direct implementation of the Military Health System (MHS) organizational reform required by the National Defense Authorization Act.
- Identification #: N/A
- Date: 9/28/2018
- Type: Memorandums
- Topics: Military Hospitals and Clinics
DHA PM 6010 13 MEPRS Volume 2
Policy
This Defense Health Agency-Procedures Manual (DHA-PM), based on the authority of References (a) and (b), and in accordance with the guidance of References (c) through (d), establishes the Defense Health Agency’s (DHA) procedures to: - a. Provide a uniform and standardized system of healthcare managerial cost accounting for the Military Health System (MHS) and MEPRS. MEPRS: (1) Provides detailed uniform performance indicators, common expense classification by work/cost center, uniform reporting of personnel utilization data by work centers, and a labor cost assignment methodology. (2) Methodology provides consistent performance data to managers responsible for healthcare delivery in support of dual Warfighter Support Operations and integrated Tri-Service healthcare missions. (3) Defines a set of functional work/cost centers, applies a uniform performance measurement system, prescribes a cost assignment methodology, and obtains reported information in standard formats for fixed Military Medical Treatment Facilities (MTFs) and DTFs. Resource and performance data must reflect the resources used in delivering healthcare services and comply with MEPRS functional work/cost center requirements. Data must be complete, accurate, and timely, and in sufficient detail to permit review and audit by management. - b. Prescribes detailed functional information for the standardized MEPRS Uniform Chart of Accounts Operational Functional Cost Codes (FCCs). - c. Cancels and along with DHA Procedures Manual “Medical Expense and Performance Reporting System (MEPRS) Procedures Manual for Fixed Military Medical and Dental Treatment Facilities: Business Rules, Volume 1,” September 27, 2018 (Reference (e)) reissues DoD 6010.13-M, “Medical Expense and Performance Reporting System for Fixed Military Medical and Dental Treatment Facilities,” April 7, 2008 (hereby canceled) (Reference (f)).
- Identification #: 6010.13
- Date: 9/27/2018
- Type: Memorandums
- Topics: Access, Cost, Quality, and Safety
DHA PM 6010 13 MEPRS Volume 1
Policy
This Defense Health Agency-Procedures Manual (DHA-PM), based on the authority of References (a) and (b), and in accordance with the guidance of References (c) through (ae), establishes the Defense Health Agency’s (DHA) procedures to: - a. Provide a uniform and standardized system of healthcare managerial cost accounting for the Military Health System (MHS) and the MEPRS. MEPRS: (1) Provides detailed uniform performance indicators, common expense classification by work center/cost center, uniform reporting of personnel utilization data by work centers, and a labor cost assignment methodology. (2) Methodology provides consistent performance data to managers responsible for healthcare delivery in support of dual Warfighter Support Operations and integrated Tri-Service healthcare missions. (3) Defines a set of functional work centers/cost centers, applies a uniform performance measurement system, prescribes a cost assignment methodology, and obtains reported information in standard formats for fixed Military Medical Treatment Facilities (MTFs) and fixed Military DTFs. Resource and performance data must reflect the resources used in delivering healthcare services and also comply with MEPRS functional work/cost center requirements. Data must be complete, accurate, and timely, and in sufficient detail to permit review and audit by management at all levels of the Health Affairs (HA) and DHA organizations. - b. Prescribes the standardized procedures, business rules, service units, allocation factors and guidelines for the uniform reporting of expense, labor/personnel, and/or output data for fixed military medical and DTFs. - c. Cancels and along with DHA Procedures Manual “Medical Expense and Performance Reporting System (MEPRS) Procedures Manual for Fixed Military Medical and Dental Treatment Facilities Uniform Chart of Accounts, Volume 2,” September 27, 2018 (Reference (e)) reissues DoD 6010.13-M, “Medical Expense and Performance Reporting System for Fixed Military MTFs and DTFs,” April 7, 2008 (hereby canceled) (Reference (f)).
- Identification #: 6010.13 Volume 1
- Date: 9/27/2018
- Type: Memorandums
- Topics: Access, Cost, Quality, and Safety
DHA IPM 18-008: Use of Medical Q Services (MQS) Contract by Military Treatment Facilities (MTFs)
Policy
This Defense Health Agency-Interim Procedures Memorandum (DHA-IPM), based on the authority of References (a) through (d): - Instructs MTFs and servicing contracting offices to use the DHA MQS contracts for the procurement of health care staffing requirements for market segments of physician, nurse, dental, and ancillary contract services in the United States and its Territories. - Is effective immediately; it must be incorporated into a forthcoming change to DHA Procedural Instruction 6025.05 (Reference (g)). This DHA-IPM will expire effective 12 months from the date of issue.
- Identification #: 18-008
- Date: 9/19/2018
- Type: DHA Interim Procedures Memorandum
- Topics: Military Hospitals and Clinics
Naval Hospital Jacksonville selected as first Navy facility to transition to DHA
Article
9/13/2018

Naval Hospital Jacksonville’s staff across six locations stands ready to make this a seamless transition for patients
Spine surgery team adds capability, improves readiness
Article
9/11/2018

The benefits of performing complex surgeries in the orthopedic spine clinic go far beyond the operating room
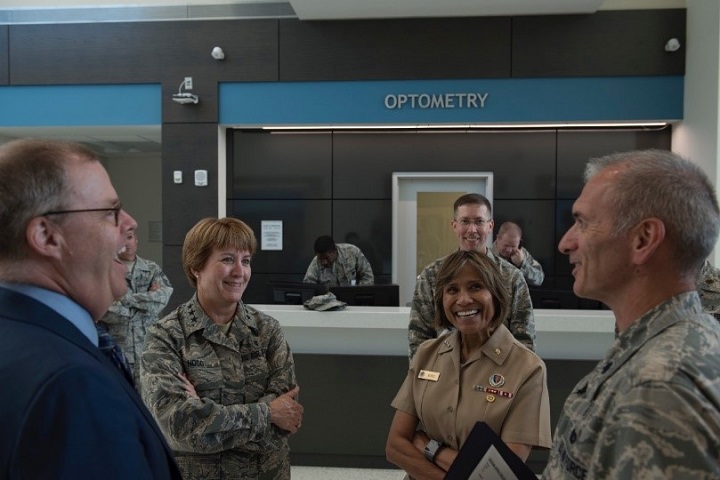
DoD, Air Force medical leaders visit JB Charleston
Article
8/13/2018
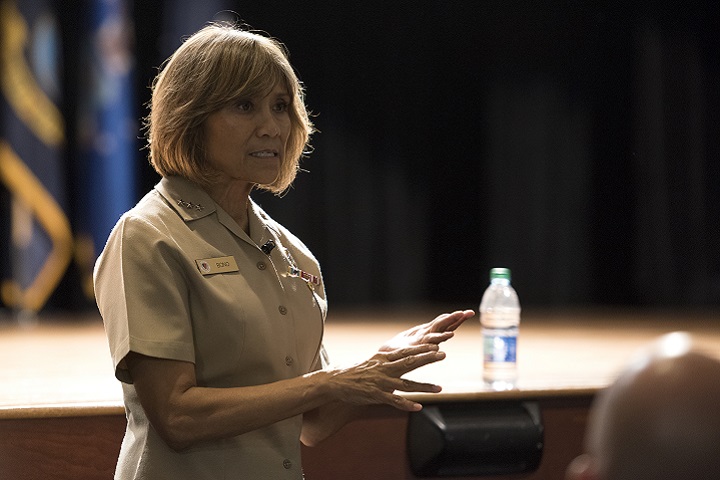
By October 2021, all military treatment facilities to include overseas facilities are scheduled to transition to DHA management
Shanahan discusses medical readiness, DHA transfer at Womack
Article
8/1/2018

The fiscal year 2017 National Defense Authorization Act transfers the administration and management of military medical treatment facilities to the DHA beginning Oct. 1, 2018





















.png)









No hay comentarios:
Publicar un comentario