
Status Update: Reducing Burden Experienced by Medicare Beneficiaries During Care Transitions
CMS is prioritizing the beneficiary’s experience through the Patient over Paperwork initiative. The agency has been working to better understand the challenges that people with Medicare face in their day-to-day lives, while navigating the complex healthcare landscape, and moving between care settings.
We used several approaches to help us better understand burdens experienced by Medicare beneficiaries:
- Formal Requests for Information
- On-site Engagement Teams
- Human-Centered Design
We then identified vehicles to help reduce burden:
- Regulatory Actions
- Communications Processes
- Education and Outreach
- eMedicare
- Health IT
- Promoting Interoperability
Throughout the summer, we spent hundreds of hours with beneficiaries, family members, caregivers, subject matter experts, and healthcare assistance organizations to hear their perspectives on difficulties accessing Medicare services. The stories we heard highlighted obstacles people face when trying to receive care. Through discussions with the Patient and Family Affinity Group and an analysis of RFI responses, call center data, and beneficiary complaint data, we determined that a deep focus on care transitions would provide the greatest benefit for beneficiaries.
What We Heard:
For twenty years a beneficiary, we will call ‘Catherine’, has been tracking her and her husband’s health records in a spreadsheet. Being both a beneficiary and a caretaker for her husband, ‘Catherine’ feels pressure to record every medication prescribed, doctor called, specialist visited, and surgery performed. She does not trust the multiple Electronic Health Record (EHR) systems and patient portals each of the seven providers maintain. She often relies on her daughter, who was a Registered Nurse to explain the benefits. ‘Catherine’ said, “Everyone now needs an advocate to get through the medical system, unless they are on top of things themselves, and very few elderly people are.”
What We Learned:
- People seek personalized and seamless transitions between care settings and providers. Many times, beneficiaries and their caregivers are bogged down by the complexity of managing health records, receiving fragmented or ad hoc treatment, and receiving guidance to act on care plans that are difficult to implement.
- People feel the standardized system does not serve their needs and that Medicare coverage is confusing. They want a system that is customer-focused, streamlined in delivery, and less restrictive in choice.
- People feel ignored by their providers and excluded from decision-making.
- Beneficiaries and their caregivers need a system that gives support and compassion for their experiences, especially when faced with high stress or time sensitive decisions.
What We Did:
Our on-site engagement team met with 46 beneficiaries and caregivers in their care settings, at their homes, and at State Health Insurance Program offices to understand healthcare services and transitions between settings. The below Beneficiary Care Activities and Transitions illustration describes the activities and types of transitions that are most challenging.

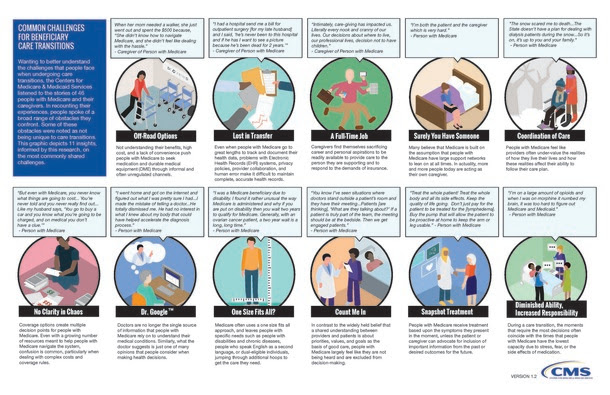
Other activities experienced by people with Medicare and their caregivers are described in the Common Challenges for Beneficiary Care Transitions visual below.
Moving Forward
CMS has been working to address the burdens that we discovered during our work to better understand the beneficiary experience. While this is a continuous effort, we have already made gains in addressing burdens. For example, we heard that people with Medicare want personalized healthcare experiences that are seamless across care settings. From our work, we have focused on empowering patients and providing them with the tools needed to make better-informed health care decisions. A number of these burdens were addressed when we finalized the Interoperability Regulations in the Inpatient Prospective Payment System (IPPS) and Long-Term Acute Care Hospital (LTCH) Prospective Payment System, and Physician Fee Schedule (PFS), designed to incentivize (1) Health Information Exchange (2) Provider to Patient Exchange of Data, and (3) Penalties for Information Blocking.
We heard numerous stories about increasing efficiencies through technology. CMS continues to promote the development of third-party applications that connect to Blue Button 2.0 through our MyHealthEData Campaign. CMS continues to explore the feasibility of supporting and encouraging Patient Navigation programs, including expansion of the Patient Navigation Pilot currently underway with the Beneficiary and Family Centered Care Quality Improvement Organizations (BFCC-QIO).





















.png)









No hay comentarios:
Publicar un comentario