
In this eighth issue of our Patients over Paperwork newsletter, we are updating you on our ongoing work to reduce administrative burden and improve the customer experience for beneficiaries. In this edition we:
Status Update: Reducing Burden Experienced by Medicare Beneficiaries During Care Transitions
CMS is prioritizing the beneficiary’s experience through the Patient over Paperwork initiative. The agency has been working to better understand the challenges that people with Medicare face in their day-to-day lives, while navigating the complex healthcare landscape, and moving between care settings.
We used several approaches to help us better understand burdens experienced by Medicare beneficiaries:
We then identified vehicles to help reduce burden:
Throughout the summer, we spent hundreds of hours with beneficiaries, family members, caregivers, subject matter experts, and healthcare assistance organizations to hear their perspectives on difficulties accessing Medicare services. The stories we heard highlighted obstacles people face when trying to receive care. Through discussions with the Patient and Family Affinity Group and an analysis of RFI responses, call center data, and beneficiary complaint data, we determined that a deep focus on care transitions would provide the greatest benefit for beneficiaries.
What We Heard:
For twenty years a beneficiary, we will call ‘Catherine’, has been tracking her and her husband’s health records in a spreadsheet. Being both a beneficiary and a caretaker for her husband, ‘Catherine’ feels pressure to record every medication prescribed, doctor called, specialist visited, and surgery performed. She does not trust the multiple Electronic Health Record (EHR) systems and patient portals each of the seven providers maintain. She often relies on her daughter, who was a Registered Nurse to explain the benefits. ‘Catherine’ said, “Everyone now needs an advocate to get through the medical system, unless they are on top of things themselves, and very few elderly people are.”
What We Learned:
What We Did:
Our on-site engagement team met with 46 beneficiaries and caregivers in their care settings, at their homes, and at State Health Insurance Program offices to understand healthcare services and transitions between settings. The below Beneficiary Care Activities and Transitions illustration describes the activities and types of transitions that are most challenging.

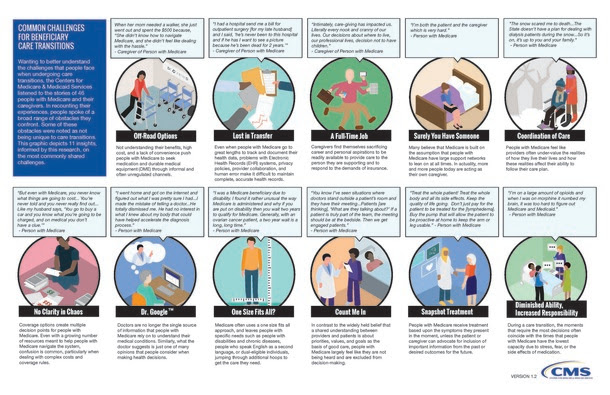
Other activities experienced by people with Medicare and their caregivers are described in the Common Challenges for Beneficiary Care Transitions visual below.
Moving Forward
CMS has been working to address the burdens that we discovered during our work to better understand the beneficiary experience. While this is a continuous effort, we have already made gains in addressing burdens. For example, we heard that people with Medicare want personalized healthcare experiences that are seamless across care settings. From our work, we have focused on empowering patients and providing them with the tools needed to make better-informed health care decisions. A number of these burdens were addressed when we finalized the Interoperability Regulations in the Inpatient Prospective Payment System (IPPS) and Long-Term Acute Care Hospital (LTCH) Prospective Payment System, and Physician Fee Schedule (PFS), designed to incentivize (1) Health Information Exchange (2) Provider to Patient Exchange of Data, and (3) Penalties for Information Blocking.
We heard numerous stories about increasing efficiencies through technology. CMS continues to promote the development of third-party applications that connect to Blue Button 2.0 through our MyHealthEData Campaign. CMS continues to explore the feasibility of supporting and encouraging Patient Navigation programs, including expansion of the Patient Navigation Pilot currently underway with the Beneficiary and Family Centered Care Quality Improvement Organizations (BFCC-QIO).
How Are We Simplifying Documentation Requirements?
CMS is working to clarify, simplify, or eliminate confusing and unnecessary documentation requirements. We continue to solicit suggestions for improvement from internal and external stakeholders. Below are the most recent changes and updates:
| ||||||||||||||||
| ||||||||||||||||
How Can I Provide Feedback?
Please send suggestions about what documentation requirements we can improve to ReducingProviderBurden@cms.
What Are We Hearing?
Additionally, we have been conducting listening sessions across the country to understand burden related to home care and hospice. Over the past month, we met with the following stakeholders:
Policy Updates
CMS Finalizes Changes to Advance Innovation, Restore Focus on Patients
Last week, the Centers for Medicare & Medicaid Services (CMS) finalized bold proposals that address provider burnout and provide clinicians immediate relief from excessive paperwork tied to outdated billing practices. The final 2019 Physician Fee Schedule (PFS) and the Quality Payment Program (QPP) rule also modernizes Medicare payment policies to promote access to virtual care, saving Medicare beneficiaries time and money while improving their access to high-quality services, no matter where they live. It makes changes to ease health information exchange through improved interoperability and updates QPP measures to focus on those that are most meaningful to positive outcomes. The rule also updates some policies under Medicare’s accountable care organization (ACO) program that streamline quality measures to reduce burden and encourage better health outcomes, although broader reforms to Medicare’s ACO program were proposed in a separate rule. This rule is projected to save clinicians $87 million in reduced administrative costs in 2019 and $843 million over the next decade.
To view the CY 2019 Physician Fee Schedule and Quality Payment Program final rule, please visit: https://s3.amazonaws.com/
For a fact sheet on the CY 2019 Physician Fee Schedule final rule, please visit: https://www.cms.gov/newsroom/
For a fact sheet on the CY 2019 Quality Payment Program final rule, please visit: https://www.cms.gov/Medicare/
For a chart on E&M payment amounts, please visit: https://www.cms.gov/sites/
CMS finalizes calendar year 2019 and 2020 payment and policy changes for Home Health Agencies and Home Infusion Therapy Supplier
The cost impact related to Outcome and Assessment Information Set (OASIS) item collection as a result of the implementation of the Patient-Driven Groupings Model, or PDGM, and finalized changes to the Home Health Quality Reporting Program (HH QRP) as outlined above, is estimated to be a net $60 million in annualized cost savings for home health agencies.
In an effort to make improvements to the health care delivery system and to reduce unnecessary burdens for physicians, CMS is eliminating the requirement that the certifying physician estimate how much longer skilled services are required when recertifying the need for continued home health care. This policy is responsive to industry concerns about regulatory burden reduction and could reduce claims denials that solely result from an estimation missing from the recertification statement. CMS estimates that this would result in annualized cost savings to certifying physicians of $14.2 million beginning in CY 2019.
For additional information about the Home Health Value-Based Purchasing Model, visit https://innovation.cms.gov/
For additional information about the Home Health Prospective Payment System, visit https://www.cms.gov/Medicare/
For additional information about the Home Health Quality Reporting Program, visit https://www.cms.gov/Medicare/
The final rule can be viewed at https://www.federalregister.
Opportunity to Provide Feedback
CMS Proposes to Lift Unnecessary Regulations and Ease Burden on Providers
In September, the Centers for Medicare and Medicaid Services (CMS) announced a proposed rule to relieve burden on healthcare providers by removing unnecessary, obsolete, or excessively burdensome Medicare compliance requirements for healthcare facilities. Collectively, CMS estimates that these updates could save healthcare providers an estimated $1.12 billion annually. Taking into account policies across rules finalized in 2017 and 2018 as well as this and other proposed rules, savings are estimated at $5.2 billion.
Many of the proposals simplify and streamline Medicare’s conditions of participation, conditions for coverage, and other requirements for participation for facilities, so they can meet health and safety standards more efficiently. This proposal ensures continued protection for patient health and safety.
CMS looks forward to feedback on the proposal and will accept comments until November 19, 2018.
Comments may be submitted electronically through our e-Regulation website https://www.cms.gov/
To learn more about the proposed rule, please visit the Federal Register: https://s3.amazonaws.com/
|





















.png)









No hay comentarios:
Publicar un comentario