
Status Update: Reducing Home Health Burden with Human Centered Design
Patients are always at the center of CMS’s work. Our Patients over Paperwork on-site engagement team recently focused on customers across the home health continuum to learn about their challenges. Over the course of 4 months, our team met with close to 100 home health agencies’ management, staff, and patients, as well as subject matter experts and home health association-representatives through interviews, observational visits, and listening sessions.
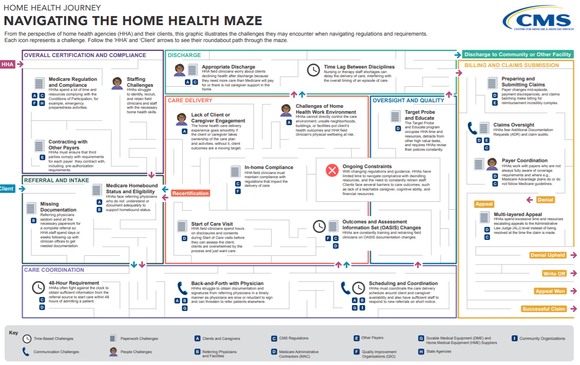
Based on the information CMS gathered, our team created an illustration to reflect the home health experience: “The Home Health Journey: Navigating the Home Health Maze” that shows key challenges home health agencies (HHAs) and their clients might face when navigating regulations and requirements.
The Value Human-Centered Design Brings to Healthcare
CMS uses human-centered design to ensure that we include our customers’ perspectives in what we learn about burden. Hearing from the customers in their home health setting was key to helping us understand their challenges, and revealed a number of areas in the home health experience for us to improve. Beyond the challenges, however, was one common theme: the mission of home health drives everyone involved. As one caregiver put it, “You’re able to see in their environment what touches them, what’s important to them, and that’s one of the things I love about home health.”
You said, We Listened
The best way for CMS to create meaningful solutions that support HHAs and the clients they serve is to understand how they operate, and how and when HHAs engage with us. That’s why we’re changing the way we inform the home health policy we write by listening to HHA employees in their workplace and experiencing a “day in the life” first hand. In the words of one home health care employee, “Communication is key and who gets caught in the middle is the patient. Policy makers need to understand how it impacts all the way down the line.”
We've turned feedback from over 2,000 individual field observations into action to address 3 of the home health concerns we heard most frequently. Here’s how we’ve worked to reduce burden in home health with customers in mind:
- Expanding caregivers’ ability to administer therapy
HHAs and caregivers told us that therapy assistants should be able to provide maintenance therapy, similar to the authority they already have to provide restorative therapy.
We listened and took action. Effective January 1, 2020, therapist assistants can now perform maintenance therapy under the home health benefit. This lets therapist assistants practice at the top of their licensure and gives HHAs the flexibility to ensure patients have access to all available levels of therapy and resources.
- Improving reporting systems
HHA staff and other personnel told us that using the Outcome and Assessment Information Set (OASIS) could be cumbersome and time consuming. One home health care worker explained, “It’s a little confusing and complex…I don’t know if it's the verbiage or how it's laid out, it's just you have to really stop and think to answer that correctly, ‘cause it just doesn’t quite make sense.”
We listened and took action. In response, with the January 1, 2020 launch of the Internet Quality Improvement and Evaluation System (iQIES), we made it easier to submit home health OASIS data. iQIES manages provider and patient information to ensure quality health care for the most vulnerable patients. This web-based system allows HHAs to work smarter through streamlined workflows, powerful reporting capabilities, and intuitive design.
3. Aligning policy, regulations, & reviews
Fear of claims denials, and resulting delays in payment, can place significant stress on any HHA. While we understand that adding requirements to a patient’s plan of care can seem burdensome, an overwhelming number of proposed rule commenters (see comments summary here: 84 FR 60551, November 8, 2019) agreed that clarifying what’s required and including it in the plan of care can reduce burden. Another way we aim to reduce administrative burden is to use the survey process instead of the claims review process to address plan of care items accidently left out.
‘Navigating The Home Health Maze’ is changing the way CMS does business
CMS is using the Navigating the Home Health Maze as an educational tool to put patients and customers at the center of our work. CMS staff is also using it to write better policies, programs, and services when they understand customers’ perspectives. We’re also excited to share it with our partners and stakeholders, letting them know we value and strive to understand our relationship with them. With tools like this, we’re better equipped to reduce burden in a meaningful way.
Snapshot: Recent Policies & Proposed Rules Aimed at Reducing Burden
Proposed Medicare Advantage and Part D changes will provide better coverage, more access and improved transparency for Medicare beneficiaries
This month, in an effort to reduce unnecessary burden, increase efficiencies, and improve the beneficiary experience, we announced that we are seeking comment on many longstanding policies on the Medicare Advantage and Part D programs. In proposed rule CMS-4190-P, we’re inviting you to comment on policies that have been adopted through sub-regulatory guidance such as the annual Call Letter and other guidance documents.
CMS will accept comments on the proposed rule through April 6, 2020.
Read the press release on the proposed rule and the 2021 Medicare Advance and Part D Advance Notice Part II.
CMS reduces psychiatric hospital burden with new survey process
Last month, we announced a streamlined state survey and certification process for psychiatric hospitals. This new process will ensure safety and quality through more holistic and efficient hospital inspections to protect patients and reduce provider burden.
For more information see the memorandum.
Fiscal year (FY) 2019 Medicare fee-for-service improper payment rate is lowest since 2010 while data points to concerns with Medicaid eligibility
Specifically, we saw a $1.82 billion reduction in estimated improper payments in the last year. This reduction is due to clarification and simplification of documentation requirements for billing Medicare under our Patients over Paperwork initiative.
Read the press release to learn more.





















.png)









No hay comentarios:
Publicar un comentario