
Management Practices to Build Evidence-Based Decision-Making Capacity for Chronic Disease Prevention in Georgia: A Case Study
COMMUNITY CASE STUDY — Volume 15 — July 12, 2018
Peg Allen, PhD1; Jean C. O’Connor, JD, DrPH2,3,4; Leslie A. Best, BSW3; Meenakshi Lakshman, MPH1; Rebekah R. Jacob, MSW, MPH1; Ross C. Brownson, PhD1,5(View author affiliations)
Suggested citation for this article: Allen P, O’Connor JC, Best LA, Lakshman M, Jacob RR, Brownson RC. Management Practices to Build Evidence-Based Decision-Making Capacity for Chronic Disease Prevention in Georgia: A Case Study. Prev Chronic Dis 2018;15:170482. DOI: http://dx.doi.org/10.5888/pcd15.170482.
PEER REVIEWED
Abstract
Background
Research shows that training can improve skills needed for evidence-based decision making, but less is known about instituting organizational supports to build capacity for evidence-based chronic disease prevention.
Community Context
The objectives of this case study were to assess facilitators and challenges of applying management practices to support evidence-based decision making in chronic disease prevention programs in the public health system in Georgia through key informant interviews and quantitatively test for changes in perceived management practices and skills through a pre–post survey.
Methods
Leadership of the chronic disease prevention section hosted a multiday training, provided regular supplemental training, restructured the section and staff meetings, led and oversaw technical assistance with partners, instituted transparent performance-based contracting, and made other changes. A 65-item online survey measured perceived importance of skills and the availability of skilled staff, organizational supports, and use of research evidence at baseline (2014) and in 2016 (after training). A structured interview guide asked about management practices, context, internal and external facilitators and barriers, and recommendations.
Capacity-Building Activities and Survey Findings
Seventy-four staff members and partners completed both surveys (70.5% response). Eleven participants also completed a 1-hour telephone interview. Interview participants deemed leadership support and implementation of multiple concurrent management practices key facilitators to increase capacity. Main challenges included competing priorities, lack of political will, and receipt of requests counter to evidence-based approaches. At posttest, health department staff had significantly reduced gaps in skills overall (10-item sum) and in 4 of 10 individual skills, and increased use of research evidence to justify interventions. Use of research evidence for evaluation, but not skills, increased among partners.
Interpretation
The commitment of leaders with authority to establish multiple management practices to help staff members learn and apply evidence-based decision-making processes is key to increased use of evidence-based chronic disease prevention to improve population health.
Background
Evidence-based decision making for chronic disease prevention (EBDM) involves complex processes, including applying program planning and quality improvement frameworks; engaging partners in assessment and decision making; adapting and implementing evidence-based policies and programs; conducting sound evaluation; and using evaluation findings to improve implementation and reach (1,2). Both individual skills and organizational supports are needed to apply and sustain EBDM processes. A literature review identified 5 domains of management practices with evidence of improving agency performance: leadership support, workforce development, organizational climate and culture, relationships and partnerships, and financial practices (3).
The Centers for Disease Control and Prevention (CDC), along with other funders, expect state public health departments to implement or contract for evidence-based approaches (4). Training in EBDM can improve skills needed to use EBDM processes (5). EBDM is also recognized as having an impact on the effectiveness of chronic disease units (6). But less is known about how to foster organizational climates that support evidence-based practice.
Community Context
The Chronic Disease Prevention Section (CDPS) of the Georgia Department of Public Health (GDPH) has about 50 staff members that help communities create policy, systems, and environmental changes to reduce risk factors for cardiovascular diseases, cancers, diabetes, asthma, and other chronic conditions, promote the healthy development of children and adolescents, and provide access to early detection and management of chronic conditions. CDPS also funds part of the cost of district health chronic disease coordinators in each of the 18 public health districts.
In fall 2013, a new chronic disease director was hired to move the section toward a coordinated chronic disease approach. To foster collaboration and information sharing to implement evidence-based approaches to reduce risk factors common across disease areas, CDPS was organized into the 4 domains of chronic disease prevention instead of disease area or funding source: epidemiology, environmental approaches, health care systems interventions, and community–clinical linkages (Figure 1). In addition, CDPS focused on the support functions necessary to support EBDM: evaluation and monitoring, administration and fiscal management, and partnerships and planning.
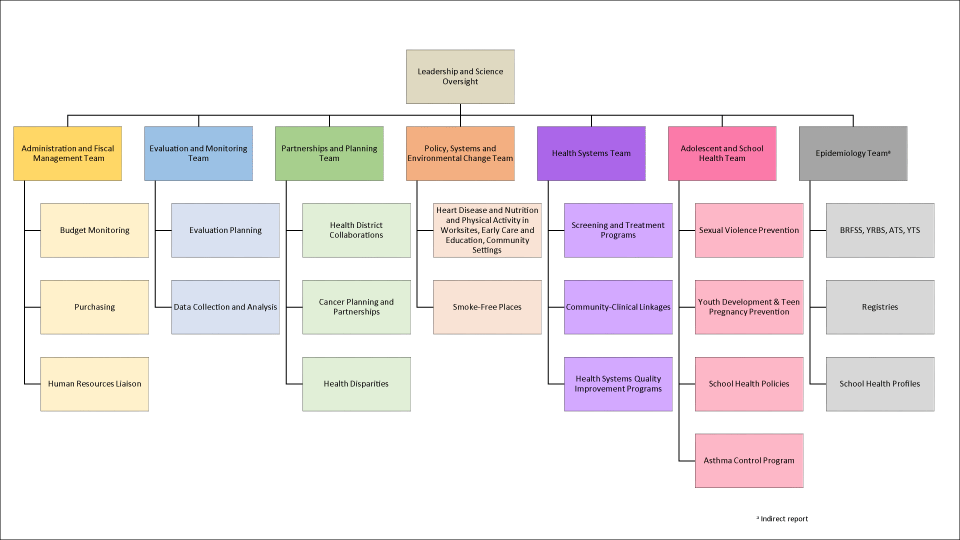
Figure 1.
Organizational framework of the Chronic Disease Prevention Section, Georgia Department of Public Health, 2017. Abbreviations: BRFSS, Behavioral Risk Factor Surveillance System; YRBS, Youth Risk Behavior Survey; ATS, Adult Tobacco Survey; YTS, Youth Tobacco Survey. [A text version of the figure is also available.]
Organizational framework of the Chronic Disease Prevention Section, Georgia Department of Public Health, 2017. Abbreviations: BRFSS, Behavioral Risk Factor Surveillance System; YRBS, Youth Risk Behavior Survey; ATS, Adult Tobacco Survey; YTS, Youth Tobacco Survey. [A text version of the figure is also available.]
In 2014, recognizing the importance of EBDM, in addition to structure, in achieving improved organizational effectiveness, CDPS also enrolled in a study to assess the impact of an EBDM training and related intervention activities (7,8). The objectives of this case study were to assess facilitators and challenges of applying management practices to support EBDM in the chronic disease prevention programs in the public health system in Georgia through key informant interviews and quantitatively test for changes in perceived management practices and EBDM skills through a pre–post survey.
Methods
Participants and data collection. In August 2014, 30 staff members from CDPS and 1 university partner attended a multiday EBDM training provided by the senior author (R.C.B.) and other faculty members and coordinated by 2 coauthors (R.R.J. and P.A). The content covered 8 modules (Figure 2), plus a ninth introductory module. Time spent on each topic varied from 90 minutes to 3 hours. Attendees participated in interactive lectures, small group exercises, and discussion. As part of a larger study (7,8), a baseline survey was conducted in June and July 2014 (before training) among all 30 professional staff members from CDPS and a purposive sample of 44 partners from other GDPH sections, district and local public health offices, universities, voluntary health agencies, community-based organizations, and other state agencies. Of 124 invited by email, 105 completed the baseline survey (84.7% response). Partners that work closely with, and are sometimes funded by, the programs were included in the survey even though they did not attend the multiday training. The CDPS had implemented management practices to ensure that funded partners were expected or required to perform the contracted work by using an EBDM approach. After the baseline survey was administered, CDPS managers discussed the survey results and lessons learned in the training and collaboratively identified a short list of next steps or problems to be solved to advance EBDM capacity and application. Of 105 participants in the baseline survey, 74 (70.5%) completed the post-training survey in April and May 2016. Five CDPS staff members and 6 partners recommended by the chronic disease director also completed 1-hour structured telephone interviews in 2016.
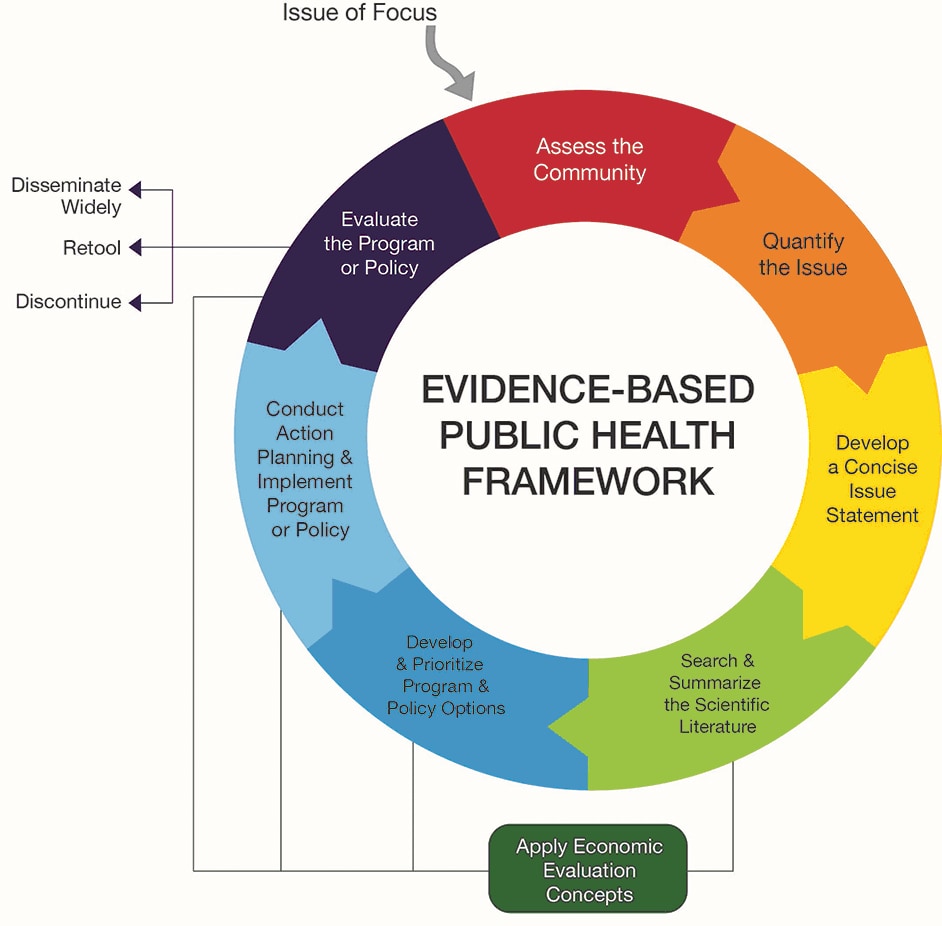
Figure 2.
Framework for training in public health evidence-based decision making. Source: Brownson et al (1). [A text version of this figure is also available.]
Framework for training in public health evidence-based decision making. Source: Brownson et al (1). [A text version of this figure is also available.]
Measures. The 65-item online survey included questions on demographics, the perceived importance of each of 10 EBDM skills (scored on an 11-point Likert scale from 0 = unimportant to 10 = very important) and the availability of agency staff members who have that skill (scored on an 11-point Likert scale from 0 = not available to 10 = very available), frequency of use of research evidence (scored on a 4-point Likert scale from 1 = seldom or never, 2 = sometimes, 3 = often, 4 = always), work unit and agency expectations and supports for EBDM (scored on a 7-point Likert scale from 1 = strongly disagree to 7 = strongly agree), and steps taken to enhance EBDM capacity (check all that apply). The measures were developed from a literature review (3) and the study team’s previous research, and validated through 5 rounds with an expert panel, cognitive response testing with 10 former chronic disease directors, and test–retest reliability with 75 state health department chronic disease staff from other states. The study framework and measures are detailed elsewhere (7,8). Structured interviews asked participants to describe management practices to support EBDM capacity and use, discuss internal and external facilitators and challenges, and recommend ways to enhance and sustain EBDM capacity and application.
Analyses. The study team conducted quantitative data management and analyses in SPSS version 24 (IBM Corp). Skill gaps for each of 10 EBDM competencies were calculated as the score for the perceived importance of the skill minus the score for the perceived availability of resources to apply the skill. The sum of the 10 skill gap scores comprised the overall EBDM skill gap. Inferential analyses included paired t tests and McNemar tests. Two study team members (P.A., M.L.) independently coded each verbatim interview transcript in NVivo version 10 (QSR International Pty Ltd) and then met to reach consensus. Coded texts were reviewed to identify themes and illustrative quotes.
Capacity-Building Activities and Survey Findings
Participant characteristics. Of the 74 survey participants that completed both baseline and post-training surveys, 30 were from CDPS. The remaining 44 surveys were completed by partners from district, local, and other state governmental agencies (38.6%), coalitions or community-based organizations (34.1%), universities (20.5%), or other organizations (6.8%). Among all participants, most were female (75.7%) and had a master’s or doctoral degree in any field (81.9%). More than one-third (37.5%) had graduate degrees in public health. Nearly half (48.6%) were at least 50 years old. Participant characteristics were similar between CDPS staff members and partners, except partners on average reported more years worked at their agency (median = 10.0 y; interquartile range [IQR], 6.5–13.5 y) and in public health (median = 16.5 y; IQR, 12.5–25.0 y) than CDPS staff members (agency, median = 5.0 y; IQR, 3.0–15.5 y; public health, median = 12.5 y; IQR, 5.0–21.5 y). The 11 participants interviewed (5 CDPS and 6 partners) had worked a median of 15.5 years (IQR, 8.0–25.0 y) in public health and a median of 5.5 years (IQR, 1.0–12.0) in their agencies.
Capacity-building activities. Initial steps after the August 2014 EBDM training included revising the staff meeting agendas to incorporate EBDM information with sharing of information across program areas; establishment of a webinar training series for staff and partners, called “Chronic Disease University,” to increase the awareness of the evidence-based strategies for chronic diseases; identifying a mechanism for staff members to have access to the scientific literature; a plan to ensure contracts funded evidence-based strategies and practices; the implementation of management support of opportunities for staff members to publish and present their work; and the addition of expectations to use EBDM approaches into CDPS staff performance plans (Table 1). Three coauthors (R.C.B., R.R.J., P.A.) provided encouragement and guidance through regular conference calls, and 3 coauthors (L.A.B., R.R.J., P.A.) reviewed program overviews. CDPS used the reviews to revise programs and communicate program plans to partners. In spring 2015, the study team provided a 2-session supplemental training on identifying and using publicly available data sources.
Concurrently, the CDPS director and her leadership team revised the section’s strategic plan in 2014; convened an advisory council with university, business, health care, and public health leaders in November 2014 that meets quarterly; reformatted staff meetings to increase cross-program sharing; prepared for a fall 2015 review by the National Association of Chronic Disease Directors that assessed core components of a successful section and provided positive feedback; developed a leadership plan from the recommendations; sought and obtained additional guidance from several CDC employees; expanded university partnerships; and supported staff in presenting at state and national conferences.
Interviews of CDPS staff members resulted in quotes that describe the EBDM capacity-building management practices instituted by the CDPS director and her leadership team (Table 2). Several participants emphasized the importance of multiple management practices and some of the structural changes in how programs were organized, stating that any single approach would not have institutionalized EBDM. Partners received several supports from CDPS: menus of evidence-based approaches in requests for local proposals, evidence information, technical assistance, training, and review of work plans. District health promotion coordinators attended annual in-person updates and monthly webinars, and CDPS posted webinar slides online. Examples of technical assistance provided by CDPS staff included helping with implementation plans and developing measures and surveys. Chronic disease indicators and resources were posted online. Partners appreciated the public access to GDPH’s central data repository and provision of additional data on request. Local coalitions received trainings from CDPS or contractors to help develop coalitions and prepare for evidence-based coalition-driven strategies. Two of 5 CDPS interview participants deemed partner training and development, and review of partner plans and progress, as the most successful aspects of CDPS’ promotion of EBDM, while the others considered leadership support as most influential.
Partners also supported CDPS by carrying out the evidence-based interventions or promoting them with other local entities, sharing success stories, modeling success for others, lending expertise to coalitions, providing training and technical assistance with local partners, and maintaining linkages with nearby universities. Some partners, especially university-based partners, “actually were a part of that call” for strengthening EBDM in Georgia and have been supportive since “they wanted the state programs to function” with more impact. Participants discussed EBDM partnering successes, including increased coalition capacity to implement policy changes, credibility, and ability to get grants, networking skills, reach, and value of evaluation.
Facilitators. Leadership support of the chronic disease director was cited repeatedly by GDPH staff and partners as the key facilitator to EBDM capacity building (Table 2). Additional facilitators discussed by GDPH staff included consistent messaging on EBDM internally and with partners; the section reorganization from a disease specific to a coordinated approach to chronic disease prevention; and evaluation staff working alongside program staff “so we know what’s working and not working and how to plan.” In addition to CDPS leadership support, partners emphasized CDPS technical assistance, relationships with local partners, and increased availability of online data from GDPH (Table 2). Partners also offered the following as facilitators: request for proposal requirements to use EBDM where “you have to have your ducks in a row beforehand”; having to report progress to GDPH or other funders; CDPS transparency in posting program budgets online and notice of funding opportunities for local public health districts; having a nearby university partner; aligning with community priorities; district health department accreditation processes where “everything is EBDM because there has to be a justification for everything that we do;” and “more frequent,” “more structured,” and “open” communication with CDPS. To participants, EBDM was not just a term, “it is in everything that we do now . . . it’s living and breathing and in my face all of the time, which is great.”
Challenges. Both partners and CDPS staff stated that competing local priorities, varied local or district leadership support, social norms, or local politics sometimes meant chronic disease prevention takes a back seat. A lack of state or local political will “sometimes means that we can’t implement what’s evidence-based practice,” depending on the “needs and appetites of the political machine.” Sometimes “we get requests that aren’t evidence-based.” Additional common challenges were time and varied EBDM familiarity and skill levels.
CDPS staff also mentioned hiring restrictions, inability to offer competitive salaries, fear of conflict with partners, resistance to change, lack of clarity from funders, societal lack of belief in prevention, a lack of alignment between partner organization goals and funding requirements, and difficulty finding partners willing to work across racial and economic lines. Partners discussed additional challenges of not having enough staff to address chronic disease prevention in the many counties each district serves, lack of public health training in local health departments, some partners not seeing where they fit into EBDM processes, lack of lead time to develop local coalitions for requests for proposals, lack of local grant writers, cultural and language barriers, little understanding among newer GDPH staff members about what districts can and cannot do, conflicts between county and state agendas, and lack of “artful” communication of evidence “in a way to get conversation going.” One interviewee said, “Folks have not always agreed that the evidence is right, especially if it goes against some held belief or value, and so that’s always a challenge.” Another one said, “And there’s also the politics of race and economics. A fair amount of that is divided along urban and rural lines, but it’s a real challenge.”
Quantitative findings. Among CDPS staff members, the largest EBDM skill gaps at baseline were in prioritization, adapting interventions, and understanding how to use economic evaluation information (Table 3). Mean perceived skill gaps significantly decreased overall (P = .02), in prioritization (P = .01), adapting interventions (P = .005), qualitative evaluation (P = .04), and action planning (P = .01). Mean perceived supervisory expectations for use of EBDM increased (P = .006), as did perceived work-unit access to staff resources for EBDM (P = .01). Use of research evidence to justify selection of interventions increased (P = .008). Among the 44 partners, use of research evidence to evaluate interventions increased (P = .03).
Commonly reported steps to improve capacity for EBDM, as reported by CDPS and partner survey participants, were informally sharing EBDM knowledge (53%), using EBDM knowledge to plan (43%) or evaluate (33%) a program, and building EBDM principles into employee performance expectations (27%).
Participant recommendations. CDPS recommendations focused on training, hiring, and educating decision makers about prevention effectiveness. Training recommendations included 1) a standardized EBDM orientation for new staff, 2) more skills-based training, not just informational trainings, and 3) more training in policy change. Staff wanted planned hiring of people experienced in policy change to continue to increase the section’s capacity to guide partners. And because of lack of belief in prevention in some areas, “it’s convincing people that prevention works. I think we have to get better at doing that.”
Partners made similar recommendations, and also wanted CDPS to 1) provide summaries of emerging issues such as e-cigarettes, 2) pool and distribute information important to communities, 3) increase interagency collaboration at the state level, 4) give as much notice as possible of upcoming proposals to allow time for local partnering in preparation, and 5) involve district staff in drafting requests for proposals. Partners also recommended hiring more district and local health promotion staff so in-person relationship building can lay the groundwork for increased local capacity to implement evidence-based practice.
Interpretation
This case study describes multiple management strategies used to build EBDM capacity in the chronic disease prevention unit of a state health department in the areas of leadership support, workforce development, partnering, and financial practices. After training and institution of management practices, self-reported EBDM skills and availability of resources for EBDM improved among CDPS staff. Use of research evidence increased among CDPS staff and partners.
Leadership support and the use of multiple management strategies rather than a single strategy emerged as the key facilitators of EBDM capacity building among interview participants. In qualitative studies in Canada, participants deemed leadership role modeling, expectations of EBDM, and provision of staff time to learn and apply EBDM processes instrumental in building EBDM capacity and use (9–11). Aarons and colleagues encourage leaders at all levels to role model and coach EBDM, pay regular attention to EBDM, stand by EBDM principles in stressful situations, direct resources to evidence-based policies and programs, acknowledge staff for applying EBDM processes, and employ and promote those experienced in EBDM or at least open to EBDM (12). Our case study showed that the chronic disease director used these and additional approaches to build capacity.
An additional strategy was the reorganization of CDPS by role instead of chronic condition, with the intent to facilitate cross-program data sharing and collaboration to better plan and implement evidence-based approaches to reduce risk factors such as obesity and tobacco use, which are common to multiple chronic diseases. In a case study of structure, chronic disease prevention staff found that collaboration was enhanced by having specialist groups meet across program areas (6). A public health department in Ontario, Canada, found that forming formal study groups across administrative boundaries facilitated ongoing communication and collaboration across programs (10). Participants in our case study reported that the formal administrative realignment facilitated communication across program areas and that it was too soon to know the full impact of the reorganization.
Workforce development was multifaceted, as recommended by Roche and colleagues (13), with ongoing supplemental webinars after the initial multiday training, internal program review, external technical assistance with partners (and at times provided by other partners), recruitment of employees with a master’s degree in public health, verbal reinforcement of EBDM principles and expectations, and incorporation into employee development plans within the constraints of the state performance review format.
Managing change with communication is critical to building EBDM capacity. Health department staff and public health leaders emphasize the importance of clear communication of EBDM principles, expectations, and processes, and sharing of information across programs (2,9–11,14–17). A health department in Ottawa, Canada, found that focusing solely on obtaining and disseminating evidence was not enough, as staff had to learn to think about different ways of approaching their jobs, which raised anxieties (10). Staff emphasized the importance of strategizing for the complexity of the changes and framing EBDM capacity building as a long-term process to allow adequate time to identify and accomplish realistic individual and organizational objectives. Supporting staff when challenged by others for EBDM processes (eg, a priority change driven by evidence) was a helpful change-management strategy in our case study and in the Ottawa health department (9). Steps taken in our case study were well aligned with recommendations for public health managers to be a change agent, use a structured process to manage change, address support and resistance to change, and recruit staff with skills to sustain change management (16). To address changes from evolving evidence and external political forces, public health change managers need skills in systems thinking, communication, organizational behavior, ethics-based approaches to achieve health equity, and policy assessment and translation (17).
The efforts to have transparent budget processes, requests for proposals, and timelines were appreciated in partner interviews. Partners wanted more lead time for requests for proposals to work through local partnerships in time to apply competitively, but they also expressed understanding of timeline constraints. Performance-based contracts ensure that resources support evidence-based planning, implementation, evaluation, and enhanced transparency in the contracting process (18).
Challenges to EBDM expressed by participants reflected barriers noted in earlier studies (4,19), where managers were recommended to acknowledge that EBDM processes are time consuming, protect staff time for EBDM processes (10,20), and create an organizational climate that promotes a balance of thinking and doing instead of all doing (10).
In addition to recommendations from interview participants, we recommend the following: 1) ongoing development among leadership teams and staff members in skills not only in EBDM but also in technical assistance, communication, strategic planning, policy development, and coalition building; 2) replication of EBDM training with nonuniversity chronic disease prevention partners; 3) long-term commitment to EBDM communication and change management; 4) enhanced engagement in participatory decision making as staff and partner skills in EBDM and communication grow; and 5) addressing health equity challenges. Health departments are directing resources to areas with poor health outcomes but lack of political will for EBDM persists in some corners. Skepticism about the effectiveness of prevention, racism and social inequality, and reluctance in some communities to partner across racial, economic, and rural/urban strata are common challenges requiring nontraditional transdisciplinary work (2).
Our case study has several limitations. Generalizability is limited because of the context of the study. The small sample sizes (30 CDPS staff members, 44 partners) made it difficult to detect significant change. The self-reported Likert items on organizational supports may not fully measure actual management practices.
Leadership support is critical for EBDM capacity building and dissemination. Commitment of leaders within agencies with authority and skills to institute multiple management practices and help staff learn and apply EBDM processes is important for the spread of evidence-based chronic disease prevention and improved population health.
Acknowledgments
This work was supported by the National Cancer Institute of the National Institutes of Health (5R01CA160327). It was also supported in part by the National Association of Chronic Disease Directors agreement no. 1612017. The authors appreciate GDPH’s support of the project and thank all the survey and interview participants from the department and partnering organizations in Georgia. At the time the work was done, Dr O’Connor was affiliated with GDPH and Ms Best was a retired chronic disease director from the Pennsylvania Department of Health who was affiliated with the National Association of Chronic Disease Directors (NACDD). Both are now affiliated with NACDD. We thank Carsten Baumann, Anjali Deshpande, and Ellen Jones for traveling to Atlanta, Georgia, to train GDPH staff. We also thank Lindsay Elliott and Alicia Manteiga for help with data collection and reports. For related research materials, please see the Prevention Research Center in St. Louis, Washington University in St. Louis website, https://prcstl.wustl.edu. Dr Ross Brownson gave permission to reprint his evidence-based decision making framework. No copyrighted materials, surveys, instruments, or tools were used in the study.
Author Information
Corresponding Author: Peg Allen, PhD, Prevention Research Center, Brown School, Washington University in St. Louis, One Brookings Dr, Campus Box 1196, St. Louis, MO 63130. Telephone: 314-935-0116. Email: pegallen@wustl.edu.
Author Affiliations: 1Prevention Research Center, Brown School, Washington University in St. Louis, St. Louis, Missouri. 2Chronic Disease Prevention Section, Georgia Department of Public Health, Atlanta, Georgia. 3National Association of Chronic Disease Directors, Atlanta, Georgia. 4The Task Force for Global Health, Decatur, Georgia. 5Department of Surgery (Division of Public Health Sciences), Alvin J. Siteman Cancer Center, Washington University School of Medicine, Washington University in St. Louis, St. Louis, Missouri.
References
- Brownson RC, Baker EA, Deshpande AD, Gillespie KN. Evidence-based public health. Third ed. New York (NY): Oxford University Press; 2018.
- Brownson RC, Fielding JE, Green LW. Building capacity for evidence-based public health. Annu Rev Public Health 2018;39:27–53. CrossRef PubMed
- Brownson RC, Allen P, Duggan K, Stamatakis KA, Erwin PC. Fostering more-effective public health by identifying administrative evidence-based practices: a review of the literature. Am J Prev Med 2012;43(3):309–19. CrossRef PubMed
- Steele CB, Rose JM, Townsend JS, Fonseka J, Richardson LC, Chovnick G. Comprehensive cancer control partners’ use of and attitudes about evidence-based practices. Prev Chronic Dis 2015;12:E113. CrossRef PubMed
- Jacob RR, Baker EA, Allen P, Dodson EA, Duggan K, Fields R, et al. Training needs and supports for evidence-based decision making among the public health workforce in the United States. BMC Health Serv Res 2014;14(1):564. CrossRef PubMed
- Alongi J. A case study examination of structure and function in a state health department chronic disease unit. Am J Public Health 2015;105(Suppl 2):e15–22. CrossRef PubMed
- Allen P, Sequeira S, Jacob RR, Hino AA, Stamatakis KA, Harris JK, et al. Promoting state health department evidence-based cancer and chronic disease prevention: a multi-phase dissemination study with a cluster randomized trial component. Implement Sci 2013;8(1):141. CrossRef PubMed
- Brownson RC, Allen P, Jacob RR, deRuyter A, Lakshman M, Reis RS, et al. Controlling chronic diseases through evidence-based decision making: a group-randomized trial. Prev Chronic Dis 2017;14:E121. CrossRef PubMed
- Ward M, Mowat D. Creating an organizational culture for evidence-informed decision making. Healthc Manage Forum 2012;25(3):146–50. CrossRef PubMed
- Peirson L, Ciliska D, Dobbins M, Mowat D. Building capacity for evidence informed decision making in public health: a case study of organizational change. BMC Public Health 2012;12(1):137.CrossRef PubMed
- Zardo P, Collie A, Livingstone C. Organisational factors affecting policy and programme decision making in a public health policy environment. Evid Policy 2015;11(4):509–27. CrossRef
- Aarons GA, Ehrhart MG, Farahnak LR, Sklar M. Aligning leadership across systems and organizations to develop a strategic climate for evidence-based practice implementation. Annu Rev Public Health 2014;35(1):255–74. CrossRef PubMed
- Roche AM, Pidd K, Freeman T. Achieving professional practice change: from training to workforce development. Drug Alcohol Rev 2009;28(5):550–7. CrossRef PubMed
- Hardy AK, Nevin-Woods C, Proud S, Brownson RC. Promoting evidence-based decision making in a local health department, Pueblo City-County, Colorado. Prev Chronic Dis 2015;12:E100.CrossRef PubMed
- Winterbauer NL, Bridger CM, Tucker A, Rafferty AP, Luo H. Adoption of evidence-based interventions in local health departments: “1-2-3 Pap NC”. Am J Prev Med 2015;49(2):309–16.CrossRef PubMed
- Thompson JM. Understanding and managing organizational change: implications for public health management. J Public Health Manag Pract 2010;16(2):167–73. CrossRef PubMed
- Erwin PC, Brownson RC. The public health practitioner of the future. Am J Public Health 2017;107(8):1227–32. CrossRef PubMed
- Honoré PA, Simoes EJ, Moonesinghe R, Kirbey HC, Renner M. Applying principles for outcomes-based contracting in a public health program. J Public Health Manag Pract 2004;10(5):451–7.CrossRef PubMed
- Jacobs JA, Dodson EA, Baker EA, Deshpande AD, Brownson RC. Barriers to evidence-based decision making in public health: a national survey of chronic disease practitioners. Public Health Rep 2010;125(5):736–42. CrossRef PubMed
- Traynor R, Dobbins M, DeCorby K. Challenges of partnership research: insights from a collaborative partnership in evidence-informed public health decision making. Evid Policy 2015;11(1):99–109. CrossRef





















.png)









No hay comentarios:
Publicar un comentario