Study explores how to repurpose HIV platform to combat NCDs
July / August 2018 | Volume 17, Number 4

Photo by Richard Lord for Fogarty
A new study details the many research
questions related to integrating
noncommunicable diseases into the HIV
care platform.
questions related to integrating
noncommunicable diseases into the HIV
care platform.
A combination of aging, long-term use of antiretroviral therapies (ART) and chronic inflammation means a growing number of people living with HIV in sub-Saharan Africa are developing non-communicable diseases (NCDs) prematurely. The global HIV response has not just provided millions with access to ART but has also made significant investments in improving health systems. But there are many considerations involved in repurposing the HIV delivery platform to tackle NCDs, which form an urgent research agenda that merits attention, according to the authors of a journal supplement devoted to the subject.
Titled “Research to Guide Practice: Enhancing HIV/AIDS Platform to Address Non-Communicable Diseases in sub-Saharan Africa ,” the collection contains a dozen open-access articles published as a supplement to AIDS, the official International AIDS Society journal. The supplement is the output from a project that Fogarty’s Center for Global Health Studies conducted with partners at NIH, CDC and USAID, with funding from NIH and PEPFAR.
Cardiovascular disease, cervical cancer, depression and diabetes are the four NCDs that are most likely to cause health problems for people living with HIV (PLHIV), according to an article that provides a systematic review and analysis of these diseases in low- and middle-income countries (LMICs). While there is little data from sub-Saharan Africa (SSA), reports indicate PLHIV are more likely to develop heart failure, stroke and embolisms than their uninfected peers. Women with HIV are at risk for human papilloma virus (HPV) disease, particularly cervical cancer, with between 10 and 40 percent having precancerous lesions and as many as 1.7 percent developing invasive cervical cancer. Depression also commonly accompanies HIV infection, contributing to greater morbidity and mortality. People who are depressed are three times more likely to be nonadherent to ART, the study also noted. There is a wide range of prevalence of diabetes among PLHIV, which reflects the variation between populations. In addition to the normal risk factors for diabetes, PLHIV also face inflammation and side effects of antiretrovirals, which may increase the likelihood for the disease.
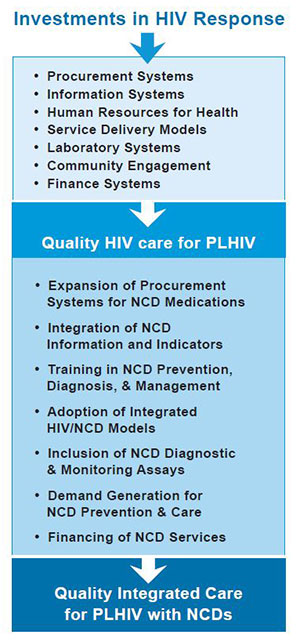
Investments in HIV response can be integrated with
noncommunicable disease (NCD) care for people
living with HIV (PLHIV), according to authors of a
journal supplement led by Fogarty’s Center for Global
Health Studies. See the full description below.
noncommunicable disease (NCD) care for people
living with HIV (PLHIV), according to authors of a
journal supplement led by Fogarty’s Center for Global
Health Studies. See the full description below.
Source: Building on the HIV platform: tackling the
challenge of noncommunicable diseases
among persons living with HIV , Figure 1
challenge of noncommunicable diseases
among persons living with HIV , Figure 1
In order to address these and other NCDs, health system deficiencies in infrastructure, human resources, medical supply chain management and program monitoring must be further strengthened, suggested authors who examined lessons learned from four SSA countries. They called for coordinated planning and action by policymakers, researchers and implementers and also noted some may perceive combining HIV and NCD client cohorts as a threat to gains made in HIV control.
An examination of global partnerships that responded to the HIV/AIDS epidemic concluded that a range of financial and technical support will also be needed to effectively combat NCDs. Economic aspects of combining NCD with HIV care programs were also studied, with authors concluding that “although integrated HIV/NCD care has many benefits, the economic justification is unproven.” Better information is needed to make the case, they said.
More data are also needed on the prevalence and incidence of NCDs among PLHIV if policymakers are to correctly assess the threat in SSA and plan investments accordingly, noted another study. Ongoing dialogue among researchers, and program implementers and policymakers is key to successful HIV/NCD integration. Another priority should be to address extensive research questions detailed in one of the papers. Issues involve service delivery models; human capacity development; research and evaluation; supply chain; financing and economics; policy, governance and leadership; health promotion; partnerships and cross-cutting issues.
Countries in SSA should look to successful HIV programs as models to confront the looming NCD health crisis. “Controlling NCDs, which represent some of the biggest killers in the world today, is feasible,” according to two of the publication’s authors, Dr. Wafaa El-Sadr, of Columbia University, and Dr. Eric Goosby, of the University of California, San Francisco. “HIV has taught us one indelible lesson: that the impossible is possible.”
More Information
- Project: Enhancing HIV/AIDS Platforms to Address NCDs in Low-resource Settings
- Publication: Research to guide practice: enhancing HIV/AIDS platform to address non-communicable diseases in sub-Saharan Africa [Open access]
Supplement to AIDS, July 1, 2018 - Related July 2018 satellite session at the International AIDS Conference, including slides: Research to guide practice: Enhancing HIV/AIDS platform to address non-communicable diseases in sub-Saharan Africa
Organized by Fogarty staff
Co-chairs: Wafaa El-Sadr and Eric Goosby
Flow chart description: Investments in HIV response includes procurement systems; information systems; human resources for health; service delivery models; laboratory systems; community engagement; finance systems. Points to quality HIV care for PLHIV includes expansion of procurement systems for NCD medications; integration of NCD information and indicators; training in NCD prevention, diagnosis & management; adoption of integrated HIV/NCD models; inclusion of NCD diagnostic & monitoring assays; demand generation for NCD prevention & care; financing of NCD services. Points to quality integrated care for PLHIV with NCDs.
To view Adobe PDF files, download current, free accessible plug-ins from Adobe's website .





















.png)









No hay comentarios:
Publicar un comentario