
Four military treatment facilities earn prestigious surgical quality awards

Navy Cmdr. Cary Schultz, a certified registered nurse anesthetist at Naval Hospital Jacksonville, monitors anesthesia levels during surgery in the operating room. “Our entire surgical team ensures that our fighting team is able to receive the treatment needed to keep them at top physical performance and ensure mission readiness,” said Schultz. The hospital was one of four MHS facilities recognized for exemplary surgical patient care in calendar year 2017. (U.S. Navy photo by Jacob Sippel)
Four military treatment facilities have been honored by the American College of Surgeons for exemplary surgical patient care in calendar year 2017. The Meritorious Awards are bestowed annually upon the top 10 percent of American College of Surgeons National Surgical Quality Improvement Program participant facilities worldwide.
“These awardees went above and beyond to meet the gold standard for quality—identifying areas for improvement to achieve benchmarked surgical outcomes,” said Vice Admiral Raquel Bono, director of the Defense Health Agency.
Winners were selected based on commendable outcomes in eight clinical areas in two separate categories, one for all cases and another for high risk cases.
The military treatment facilities recognized for all cases were David Grant Medical Center, Fairfield, California; Darnall Army Medical Center, Fort Hood, Texas; Naval Hospital Jacksonville, Florida; and Naval Medical Center Portsmouth, Virginia. Both David Grant Medical Center and Naval Medical Center Portsmouth also received Meritorious Distinction recognition for outcomes in high-risk cases.
The four facilities’ surgical outcomes were in the top 10 percent of all participants, sharing this distinction with 83 hospitals worldwide. David Grant Medical Center, honored in both categories, was recognized for the third year in a row.
Participation in the National Surgical Quality Improvement Program or NSQIP is voluntary and open to any hospital wanting to improve surgical outcomes. The Military Health System has enrolled 46 hospitals, which is all of its eligible military treatment facilities, in the program.
"We are proud of the four facilities recognized for their excellence in surgical quality," said Dr. Paul R. Cordts, Deputy Assistant Director of Medical Affairs, Defense Health Agency. All of our hospitals are strengthened by this partnership with the American College of Surgeons and the value of comparing our performance to civilian healthcare leaders."
The program, developed by surgeons for surgeons, requires each hospital to submit data into a centralized database for rigorous statistical analysis, thus enabling benchmarking against similar hospitals with similar patients. Surgeon-nurse co-led teams at each facility collect the data from patients’ medical charts on their perioperative experience, capturing surgical complication rates based on 30-day patient outcomes. Teams use their data to evaluate outcomes and determine actionable improvements, creating a culture of continuous quality improvement.
The Department of Defense supports a NSQIP collaborative among the military treatment facility teams, providing an opportunity to share successes and challenges across facilities, and facilitating mentoring, education, and networking opportunities for the staff. A Steering Panel provides leadership and oversight of the collaborative with representatives from the Defense Health Agency and each service medical branch.
“The teams are dedicated to improvement,” said Ret. Navy Capt. Mollie Mullen, Advisor for Clinical Quality, Directorate for Surgical Services at the Naval Medical Center in San Diego; Mullen also co-chairs the NSQIP Steering Panel. “They are committed to very rigorous data collection, review, and process improvement that has led to a culture of high quality patient care.”
Medical team saves newborn’s life
Article
1/15/2019

Staff quickly respond to the obstetrical emergency via an emergency cesarean section
Surgeons share secrets of residency success
Article
12/11/2018

Madigan's general surgery residents have passed the exam for board certification on their first attempt at a nation-topping rate of 97.6 percent
DHA IPM 18-012: The DoD Medical Ethics Program (DoDMEP) in the Military Health System (MHS)
Policy
This Defense Health Agency-Interim Procedures Memorandum (DHA-IPM), based on the authority of References (a) through (c), and in accordance with the guidance of References (d) through (k), establishes Defense Health Agency’s (DHA) procedures that: • Apply to Active Duty Service members, namely Active Component members and Reserve Component members on active duty for a period of more than 30 days, who, hereafter, are referred to collectively as Active Duty Service members (References (e) and (f)). • Establish a set of common guidelines, standards, and procedures governing the DoDMEP for military health care personnel in all locations. • Outline implementing procedures for DHA collaboration with the DoDMEP office, to be known as the DoD Medical Ethics Center (DMEC), which is to operate under the direction of the President of the Uniformed Services University of the Health Sciences (USUHS). • Implement guidance for the DoD mission, vision, guiding principles of the DoDMEP (DMEC) as set forth in Reference (g) and delineate areas of responsibility between the DHA and USUHS, including: o The provision of medical ethics education and training (E&T) to health care providers and other health care personnel; o Creation and maintenance of a DMEC portal; and o Medical ethics consultation services to MHS health care personnel across all settings. • This DHA-IPM is effective immediately and will expire effective 12 months from the date of issue.
- Identification #: 18-012
- Date: 10/9/2018
- Type: DHA Interim Procedures Memorandum
- Topics: Access, Cost, Quality, and Safety
DHA PM 6010 13 MEPRS Volume 2
Policy
This Defense Health Agency-Procedures Manual (DHA-PM), based on the authority of References (a) and (b), and in accordance with the guidance of References (c) through (d), establishes the Defense Health Agency’s (DHA) procedures to: - a. Provide a uniform and standardized system of healthcare managerial cost accounting for the Military Health System (MHS) and MEPRS. MEPRS: (1) Provides detailed uniform performance indicators, common expense classification by work/cost center, uniform reporting of personnel utilization data by work centers, and a labor cost assignment methodology. (2) Methodology provides consistent performance data to managers responsible for healthcare delivery in support of dual Warfighter Support Operations and integrated Tri-Service healthcare missions. (3) Defines a set of functional work/cost centers, applies a uniform performance measurement system, prescribes a cost assignment methodology, and obtains reported information in standard formats for fixed Military Medical Treatment Facilities (MTFs) and DTFs. Resource and performance data must reflect the resources used in delivering healthcare services and comply with MEPRS functional work/cost center requirements. Data must be complete, accurate, and timely, and in sufficient detail to permit review and audit by management. - b. Prescribes detailed functional information for the standardized MEPRS Uniform Chart of Accounts Operational Functional Cost Codes (FCCs). - c. Cancels and along with DHA Procedures Manual “Medical Expense and Performance Reporting System (MEPRS) Procedures Manual for Fixed Military Medical and Dental Treatment Facilities: Business Rules, Volume 1,” September 27, 2018 (Reference (e)) reissues DoD 6010.13-M, “Medical Expense and Performance Reporting System for Fixed Military Medical and Dental Treatment Facilities,” April 7, 2008 (hereby canceled) (Reference (f)).
- Identification #: 6010.13
- Date: 9/27/2018
- Type: Memorandums
- Topics: Access, Cost, Quality, and Safety
DHA PM 6010 13 MEPRS Volume 1
Policy
This Defense Health Agency-Procedures Manual (DHA-PM), based on the authority of References (a) and (b), and in accordance with the guidance of References (c) through (ae), establishes the Defense Health Agency’s (DHA) procedures to: - a. Provide a uniform and standardized system of healthcare managerial cost accounting for the Military Health System (MHS) and the MEPRS. MEPRS: (1) Provides detailed uniform performance indicators, common expense classification by work center/cost center, uniform reporting of personnel utilization data by work centers, and a labor cost assignment methodology. (2) Methodology provides consistent performance data to managers responsible for healthcare delivery in support of dual Warfighter Support Operations and integrated Tri-Service healthcare missions. (3) Defines a set of functional work centers/cost centers, applies a uniform performance measurement system, prescribes a cost assignment methodology, and obtains reported information in standard formats for fixed Military Medical Treatment Facilities (MTFs) and fixed Military DTFs. Resource and performance data must reflect the resources used in delivering healthcare services and also comply with MEPRS functional work/cost center requirements. Data must be complete, accurate, and timely, and in sufficient detail to permit review and audit by management at all levels of the Health Affairs (HA) and DHA organizations. - b. Prescribes the standardized procedures, business rules, service units, allocation factors and guidelines for the uniform reporting of expense, labor/personnel, and/or output data for fixed military medical and DTFs. - c. Cancels and along with DHA Procedures Manual “Medical Expense and Performance Reporting System (MEPRS) Procedures Manual for Fixed Military Medical and Dental Treatment Facilities Uniform Chart of Accounts, Volume 2,” September 27, 2018 (Reference (e)) reissues DoD 6010.13-M, “Medical Expense and Performance Reporting System for Fixed Military MTFs and DTFs,” April 7, 2008 (hereby canceled) (Reference (f)).
- Identification #: 6010.13 Volume 1
- Date: 9/27/2018
- Type: Memorandums
- Topics: Access, Cost, Quality, and Safety
HRO Corner: DoD PSP Collaborates with MHS Community to Standardize Dental Patient Safety
Article
9/4/2018

The Military Health System’s first-ever dental guidebook supports frontline staff, standardization of dental patient safety across the organization.
Feature: Improving Patient Safety by Improving Health Literacy Transparency
Article
9/4/2018

The Military Health System’s sharing of quality, patient safety and access information online empowers patients to ask questions and improve their health literacy
Patient Safety in Action: Huddles around Whiteboards Help Airmen See the Big Picture
Article
9/4/2018
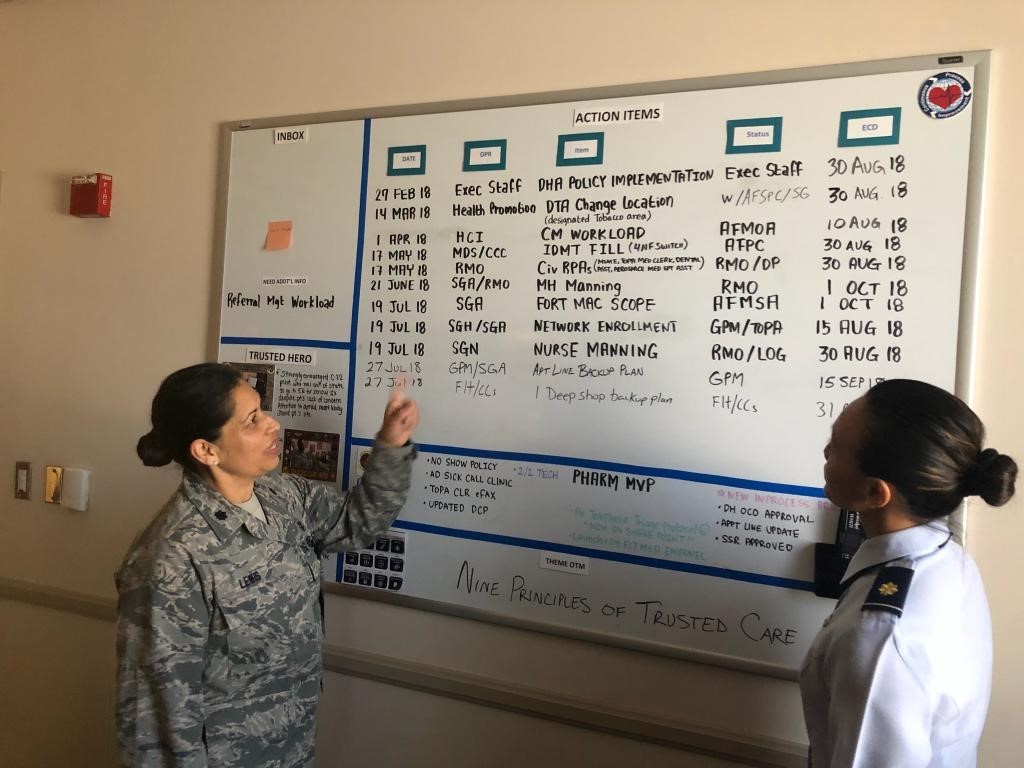
Air Force military treatment facilities use visual management boards to improve teamwork and communication across frontline staff and leadership.
DoD PSP Treasure Chest: July/August Edition
Article
7/1/2018

July/August 2018 edition of the Department of Defense Patient Safety Program Treasure Chest
Two MHS providers achieve top scores in the patient experience survey
Article
6/4/2018

The MHS recently published its annual “Best of the Best” report on medical providers
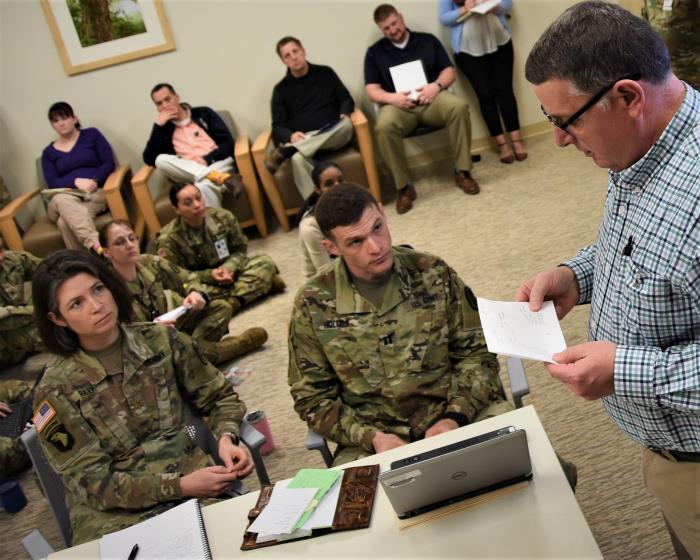
HRO Corner: Army Focuses on Leadership, Collaboration to Improve Patient Safety
Article
5/1/2018

The Army’s high reliability efforts focuses on continuous learning and leadership engagement.
DoD PSP Treasure Chest: May/June Edition
Article
5/1/2018

May/June 2018 edition of the Department of Defense Patient Safety Program Treasure Chest
Patient Safety in Action: Irwin Army Community Hospital Builds a Tiered Safety Briefing Structure
Article
5/1/2018
In less than a year, leaders at Irwin Army Community Hospital developed and launched a tiered leadership safety briefing that has improved the culture of safety.
Feature Patient Safety Awareness Week 2018 around the DoD
Article
5/1/2018

Military Treatment facilities worldwide were “United for Patient Safety” in a variety of ways during Patient Safety Awareness Week.
DoD Patient Safety Program 2018 May Learning Update
Publication
5/1/2018





















.png)









No hay comentarios:
Publicar un comentario