
Patient Safety Primer
Wrong-Site, Wrong-Procedure, and Wrong-Patient Surgery
Background
Few medical errors are as vivid and terrifying as those that involve patients who have undergone surgery on the wrong body part, undergone the incorrect procedure, or had a procedure intended for another patient. These "wrong-site, wrong-procedure, wrong-patient errors" (WSPEs) are rightly termed never events—errors that should never occur and indicate serious underlying safety problems.
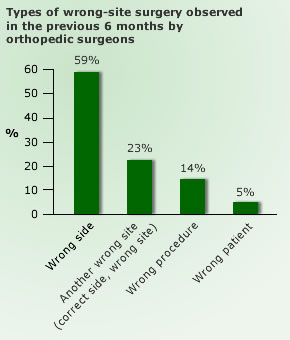
Wrong-site surgery may involve operating on the wrong side, as in the case of a patient who had the right side of her vulva removed when the cancerous lesion was on the left, or the incorrect body site. One example of surgery on the incorrect site is operating on the wrong level of the spine, a surprisingly common issue for neurosurgeons. A classic case of wrong-patient surgery involved a patient who underwent a cardiac procedure intended for another patient with a similar last name.
While much publicity has been given to these high-profile cases of WSPEs, these errors are in fact relatively rare. A seminal study estimated that such errors occur in approximately 1 of 112,000 surgical procedures, infrequent enough that an individual hospital would only experience one such error every 5–10 years. However, this estimate only included procedures performed in the operating room; if procedures performed in other settings (for example, ambulatory surgery or interventional radiology) are included, the rate of such errors may be significantly higher. One study using Veterans Affairs data found that fully half of WSPEs occurred during procedures outside of the operating room.
Preventing Wrong-Site, Wrong-Procedure, and Wrong-Patient Surgery
Early efforts to prevent WSPEs focused on developing redundant mechanisms for identifying the correct site, procedure, and patient, such as "sign your site" initiatives, that instructed surgeons to mark the operative site in an unambiguous fashion. However, it soon became clear that even this seemingly simple intervention was problematic. An analysis of the United Kingdom's efforts to prevent WSPEs found that, although dissemination of a site-marking protocol did increase use of preoperative site marking, implementation and adherence to the protocol differed significantly across surgical specialties and hospitals, and many clinicians voiced concerns about unintended consequences of the protocol. In some cases, there was even confusion over whether the marked site indicates the area to be operated on, or the area to be avoided. Site marking remains a core component of The Joint Commission's Universal Protocol to prevent WSPEs.
Root cause analyses of WSPEs consistently reveal communication issues as a prominent underlying factor. The concept of the surgical timeout—a planned pause before beginning the procedure in order to review important aspects of the procedure with all involved personnel—was developed to improve communication in the operating room and prevent WSPEs. The Universal Protocol also specifies use of a timeout prior to all procedures. Although initially designed for operating room procedures, timeouts are now required before any invasive procedure. Comprehensive efforts to improve surgical safety have incorporated timeout principles into surgical safety checklists; while these checklists have been proven to improve surgical and postoperative safety, the low baseline incidence of WSPEs makes it difficult to establish that a single intervention can reduce or eliminate WSPEs.
It is worth noting, however, that many cases of WSPEs would still occur despite full adherence to the Universal Protocol. Errors may happen well before the patient reaches the operating room, a timeout may be rushed or otherwise ineffective, and production pressures may contribute to errors during the procedure itself. Ultimately, preventing WSPEs depends on the combination of system solutions, strong teamwork and safety culture, and individual vigilance.
Current Context
Wrong-patient, wrong-site, and wrong-procedure errors are all considered never events by the National Quality Forum, and are considered sentinel events by The Joint Commission. In February 2009, the Centers for Medicare and Medicaid Services (CMS) announced that hospitals will not be reimbursed for any costs associated with WSPEs. (CMS has not reimbursed hospitals for additional costs associated with many preventable errors since 2007.)





















.png)









No hay comentarios:
Publicar un comentario