
AHRQ Stats: MRSA in California
In 2013, 8 percent of patients in California with MRSA (methicillin-resistant Staphylococcus aureus) acquired the infection during a hospital stay. (Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project Statistical Brief #212, Hospital-, Health Care-, and Community-Acquired MRSA: Estimates From California Hospitals, 2013.)
Hospital-, Health Care-, and Community-Acquired MRSA: Estimates From California Hospitals, 2013 #212

|
Janet P. Sutton, Ph.D., and Claudia A. Steiner, M.D., M.P.H. Introduction Methicillin-resistant Staphylococcus aureas (MRSA) is a bacterium that is resistant to many of the most commonly prescribed beta-lactam antibiotics, including penicillin, amoxycillin, oxacillin, and methicillin. Severe cases of MRSA may result in endocarditis, osteomyelitis, septicemia, or even death. Each year MRSA accounts for approximately 11,000 deaths in the United States.1 Costs associated with a MRSA infection are high, with an average hospital length of stay of 10 days and average hospital costs of $14,000. The average length of stay and hospital costs associated with MRSA are approximately 2 times higher than those of other hospital stays.2 MRSA typically is classified as hospital acquired; health care acquired, community onset; or community acquired, community onset. Hospital-acquired MRSA usually is the result of a nosocomial infection, often acquired following a surgical or invasive medical procedure during a hospital stay. Health care-acquired MRSA develops outside the hospital while the patient is in the community and has had recent contact or received treatment in a health care facility, such as an inpatient hospital, ambulatory surgical center, dialysis center, or nursing facility.3 Community-acquired MRSA occurs among community-dwelling individuals without recent hospitalization or encounters with the health care system. Centers for Disease Control and Prevention data indicate that between 2005 and 2011 the incidence of hospital-acquired MRSA dropped by more than 50 percent. During this same period the incidence of community-acquired MRSA decreased by only 5 percent.4 This HCUP Statistical Brief examines inpatient hospital stays with MRSA in California in 2013. Inpatient stays are categorized by clinical condition associated with MRSA—pneumonia, septicemia, cellulitis or skin ulcers, complications following surgery or medical care, and other clinical conditions. Patients with a MRSA-associated hospital admission who acquired the infection during the course of the hospitalization are then compared with those who acquired the infection following receipt of treatment or care in a health care facility in the past 90 days or who acquired the infection in the community. Health care facilities include inpatient hospital settings, emergency departments, and ambulatory surgery facilities. Differences greater than 10 percent are noted in the text. Findings Hospital inpatient stays with MRSA, California, 2013 Figure 1 presents data on the percentage of MRSA-related inpatient stays in California hospitals by clinical condition. If a patient had more than one stay in the year, each inpatient stay is counted separately. |
|
Figure 1. MRSA-associated inpatient stays in California hospitals by clinical condition associated with MRSA, 2013
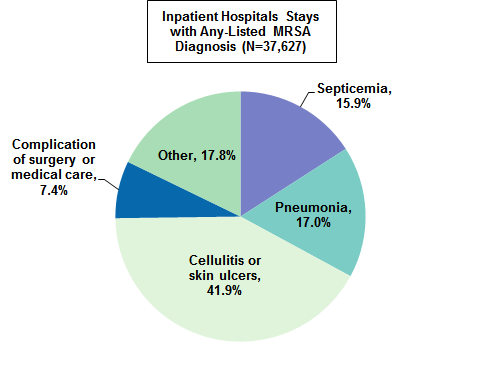
Abbreviation: MRSA, methicillin-resistant Staphylococcus aureas
Source: Agency for Healthcare Research and Quality (AHRQ), Center for Delivery, Organization, and Markets, Healthcare Cost and Utilization Project (HCUP), State Inpatient Database (SID), California, 2013
Figure 1 is a pie chart that shows the percentage of MRSA-associated hospital stays in California in 2013 by clinical condition associated with MRSA. Septicemia: 15.9; pneumonia: 17.0; cellulitis and skin ulcers: 41.9; complications of surgery or medical care: 7.4; other: 17.8.
|
Figure 2 displays the number of single and multiple hospitalizations among patients with a MRSA-associated admission that occurred during 2013. The subsequent analyses track patients across multiple MRSA hospitalizations. Patients are counted once rather than counting each hospital stay. |
Figure 2. Percentage distribution of the number of MRSA-associated hospital stays among patients with at least one MRSA admission in California, 2013
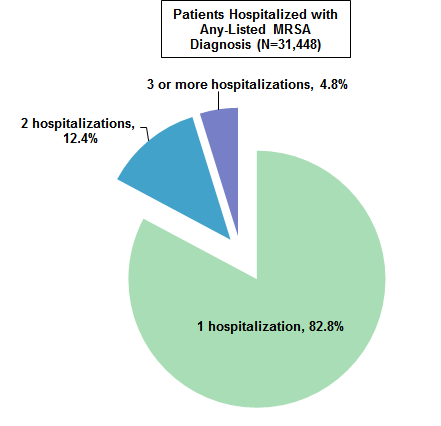
Abbreviation: MRSA, methicillin-resistant Staphylococcus aureas
Note: Patients were categorized according to their total number of inpatient stays with a MRSA diagnosis with no restriction on the number of days between MRSA admissions. Source: Agency for Healthcare Research and Quality (AHRQ), Center for Delivery, Organization, and Markets, Healthcare Cost and Utilization Project (HCUP), State Inpatient Database (SID), California, 2013
Figure 2 is a pie chart that shows the percentage distribution of MRSA-associated hospital stays among patients with at least one MRSA admission in California in 2013. Patients with 1 MRSA hospitalization: 82.8; 2 MRSA hospitalizations: 12.4; 3+ MRSA hospitalizations: 4.8.
|
Table 1 presents data on the demographic characteristics of the 31,448 patients who were hospitalized with a MRSA diagnosis in 2013. |





















.png)









No hay comentarios:
Publicar un comentario