
Patient Safety Primer
Reporting Patient Safety Events
Background
Patient safety event reporting systems are ubiquitous in hospitals and are a mainstay of efforts to detect patient safety events and quality problems. Incident reporting is frequently used as a general term for all voluntary patient safety event reporting systems, which rely on those involved in events to provide detailed information. Initial reports often come from the frontline personnel directly involved in an event or the actions leading up to it (e.g., the nurse, pharmacist, or physician caring for a patient when a medication error occurred), rather than management or patient safety professionals. Voluntary event reporting is therefore a passive form of surveillance for near misses or unsafe conditions, in contrast to more active methods of surveillance such as direct observation of providers or chart review using trigger tools. The Patient Safety Primer Detection of Safety Hazards provides a detailed discussion of other methods of identifying errors and latent safety problems.
Characteristics of Incident Reporting Systems
An effective event reporting system should have four key attributes:
| Box. Key Components of an Effective Event Reporting System |
|---|
|
While traditional event reporting systems have been paper based, technological enhancements have allowed the development of Web-based systems and systems that can receive information from electronic medical records. Specialized systems have also been developed for specific settings, such as the Intensive Care Unit Safety Reporting System and systems for reporting surgical and anesthesia-related errors.
Voluntary event reporting systems need not be confined to a single hospital or organization. The United Kingdom's National Patient Safety Agency maintains the National Reporting and Learning System, a nationwide voluntary event reporting system, and the MEDMARX voluntary medication error reporting system in the U.S. has led to much valuable research.
The advantages of voluntary event reporting systems include their relative acceptability and the involvement of frontline personnel in identifying safety hazards for the organization. Because event reports usually are submitted by personnel involved in the events themselves, these caregivers may have legitimate concerns about the effects reporting will have on their performance records. Voluntary event reporting systems are generally confidential, in that the identity of the reporter is known, but legal protection is provided unless professional misconduct or criminal acts took place. Some systems, such as the ICU Safety Reporting System, are entirely anonymous–neither the patient nor the reporter can be identified.
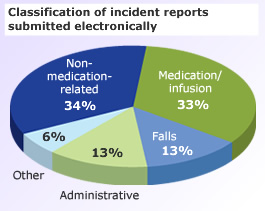
Studies of electronic hospital event reporting systems generally show that medication errors and patient falls are among the most frequently reported events.
Source: Milch CE, Salem DN, Pauker SG, Lundquist TG, Kumar S, Chen J. Voluntary electronic reporting of medical errors and adverse events. J Gen Intern Med. 2006;21:165-170. [go to PubMed]
Limitations of Event Reporting
The limitations of voluntary event reporting systems have been well documented. Event reports are subject to selection bias due to their voluntary nature. Compared with medical record review and direct observation, event reports capture only a fraction of events and may not reliably identify serious events. The spectrum of reported events is limited, in part due to the fact that physicians generally do not utilize voluntary event reporting systems.
Source: Evans SM, Berry JG, Smith BJ, et al. Attitudes and barriers to incident reporting: a collaborative hospital study. Qual Saf Health Care. 2006;15:39-43. [go to PubMed]
A 2008 study of over 1600 U.S. hospitals evaluated their event reporting systems using the criteria above (Box) and concluded that according to these standards, most hospitals do not maintain effective event reporting systems. In addition to lack of physician reporting, most hospitals surveyed did not have robust processes for analyzing and acting upon aggregated event reports. Failure to receive feedback after reporting an event is a commonly cited barrier to event reporting by both physicians and allied health professionals.
While event reports may highlight specific concerns that are worthy of attention, they do not provide insights into the epidemiology of safety problems. In a sense, event reports supply the numerator (the number of events of a particular type–and even here, this number only reflects a fraction of all such events) but do not supply the denominator (the number of patients vulnerable to such an event) or the number of "near misses." Event reports therefore provide a snapshot of safety issues, but on their own, cannot place the reported problems into the appropriate institutional context. One way to appreciate this issue is to observe that some institutions celebrate an increase in event reports as a reflection of a "reporting culture," while others celebrate a reduction in event reports, assuming that such a reduction is due to fewer events.
Using Event Reports to Improve Safety
A 2016 article contrasted event reporting in health care with event reporting in other high-risk industries (such as aviation), pointing out that event reporting systems in health care have placed too much emphasis on collecting reports instead of learning from the events that have been reported. Event reporting systems are best used as a way of identifying issues that require further, more detailed investigation. While event reporting utilization can be a marker of a positive safety culture within an organization, organizations should resist the temptation to encourage event reporting without a concrete plan for following up on reported events. A PSNet perspective described a framework for incorporating voluntary event reports into a cohesive plan for improving safety. The framework emphasizes analysis of the events and documenting process improvements arising from event analysis, rather than encouraging event reporting for its own sake.
Current Context
At the national level, regulations implementing the Patient Safety and Quality Improvement Act became effective on January 19, 2009. The legislation provides confidentiality and privilege protections for patient safety information when health care providers work with new expert entities known as Patient Safety Organizations (PSOs). Health care providers may choose to work with a PSO and specify the scope and volume of patient safety information to share with a PSO. Because health care providers can set limits on the ability of PSOs to use and share their information, this system does not follow the pattern of traditional voluntary reporting systems. However, health care providers and PSOs may aggregate patient safety event information on a voluntary basis, and AHRQ will establish a network of patient safety databases that can receive and aggregate nonidentifiable data that are submitted voluntarily. AHRQ has also developed Common Formats—standardized definitions and reporting formats for patient safety events—in order to facilitate aggregation of patient safety information. Since their initial release in 2009, the Common Formats have been updated and expanded to cover a broad range of safety events.
As all hospitals are required to maintain a confidential event reporting system, existing voluntary reporting systems have a shared interest in developing ways to compare and benchmark safety data. AHRQ will encourage use of the initial set of Common Formats by hospitals in their internal event reporting systems and encourage other voluntary reporting systems to consider adopting the Common Formats as well. Future Common Formats will address other sites of care and other stages of the improvement process (such as forms for reporting root cause analyses).





















.png)









No hay comentarios:
Publicar un comentario